Abstract
Abstract 2005
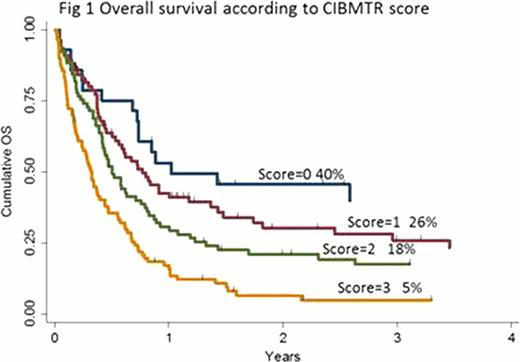
The dismal prognosis of AML patients undergoing allogeneic stem cell transplantation not in complete remission at time of conditioning poses challenging clinical decisions. In these patients, a recent, large retrospective analysis conducted by the CIBMTR showed that a myeloablative HCST can induce an overall 19% long term survival. Based on five adverse pretransplantation variables (first CR duration less than 6 months, circulating blasts, donor other than HLA-identical sibling, Karnofsky or Lansky score less than 90, and poor-risk cytogenetics) this analysis allowed to set up a pre-HSCT score (from 0 to ≥3) able to identify four risk groups defining a 3-years overall survival (OS) probability ranging from 6% up to 42% (Duval M, JCO 2010). However, this CIBMTR analysis was limited to patients with the following characteristics: a) de novo AML or secondary AML to a previous MDS b) patients receiving a TBI or busulfan based myeloablative conditioning regimens (MAC) and a BM or PB derived stem cell graft. Here we report data obtained in Italy in a similar cohort of AML patients that also included those receiving a reduced-intensity conditioning (RIC) regimen and those grafted with a cord blood unit.
We retrospectively analyzed data reported to the GITMO registry by 20 Italian centers on 523 AML patients who underwent a first HSCT being not in complete remission (CR) at time of conditioning, between 1999 and 2010. The median age at HSCT was 47,6 years (18–72), the male/female ratio 50%. At diagnosis 71,5% were de novo AML, 23% were secondary to a previous MDS/CMML, while in 5,5% the AML was therapy related or secondary to a previous CMN. Before HSCT conditioning, patients were primary refractory (PIF) in 34%, in first or subsequent untreated relapse in 45% and 16%, respectively or an untreated MDS to AML evolution in 5%. Before HSCT, 79% of PIF received ≥2 chemotherapy cycles and for relapsed patients the duration of the first CR was < 6 months in 50%. An intermediate-II or adverse karyotype was detected in 43% of patients, a greater than 25% marrow blast infiltration or any level of peripheral blood (PB) blasts was found in 53% and a pre-HSCT Karnofsky score less than 90 was present in 38%. The stem cell source was the PB in 65%, the bone marrow in 28% and the cord blood in 6%. Donors were HLA identical sibling or matched unrelated donor in 69%, a family or unrelated mismatched in 25% and a cord blood unit in 6%. Anti-CMV antibodies were present in 87% of patients and in 66% of the donors, while donor-recipient pair were sex-matched in 50% of the cases. More than 60% patients received a MAC and 37% a RIC program.
After HSCT, a myeloid and platelets engraftment was achieved in 87% of patients after a median of 17 (9–63) and 18 (2–117) days, respectively. Acute GVHD (grade ≥2 60%) was registered in 46% while chronic GVHD developed in 31%. The median follow up of the whole patients cohort was 5,36 months (0.09–133) while that of survivors was 26 months (1–133) with 96 patients alive and 77 leukemia-free. A multivariate analysis identified 7 pre-HSCT adverse variables that significantly influenced survival: an AML secondary to a previous chronic myeloproliferative neoplasm or a therapy related AML (HR 1,83, 95%CI 1,14–2,96, p 0,013), a relapsed AML with a first CR duration < 6 months (HR 1,39, 95%CI 1,06–1,82, p 0,018), an AML with a PIF after ≥2 chemotherapy cycles pre-HSCT (HR 1,74, 95%CI 1,11–2,74, p 0,016), an intermediate II/adverse cytogenetics (HR1,71, 95%CI 1,11–2,62, p 0,015), BM blasts ≥25% or any level of PB at HSCT (HR 1,65, 95%CI, 1,31–2,07, p 0.000) and a mismatched related/unrelated donor (HR 1,56, 95%CI, 1,23–1,98, p 0.000). At 3-years, the OS and LFS of our patients was 16% and 21%. Interestingly, when applied to our results, the CIBMTR score was fully validated in our patients with a 3-year survival rate decreased from 40% (score 0, HR1) to 26% (score 1, HR 1,39; 95%CI 0.88–2,12, p 0,142), to 18% (score 2, HR 1,58; 95%CI 1–2,43, p 0,04) to 5% (score 3, HR 2,83; 95%CI 1,71–4,16, p 0,000) (Figure 1).
Our results confirm that a) HSCT is a potentially curative option for a significant proportion of AML patients undergoing transplant not in remission, b) these patients may benefit from either a MAC or a RIC conditioning regimens and c) the CIBMTR score applied to this poor prognosis AML cohort is a useful tool for patient counseling and for planning the HSCT activity.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal