Abstract
Abstract 1780
Biological features related to the development of autoimmune hemolytic anemia (AHIA) in patients with chronic lymphocytic leukemia (CLL) are crucial insights in the understanding of the pathogenesis of autoimmune phenomena in the course of the disease.
We retrospectively analyzed 585 CLL patients with available immunoglobulin heavy-chain variable (IGHV) gene status and B-cell receptor (BCR) configuration (HCDR3). Of them, 73 developed AIHA. The clinical characteristics at CLL diagnosis and follow-up were available in all patients, while cytogenetic analysis at the time of diagnosis was available in 409 patients.
Occurrence of AIHA was significantly associated with an IGHV unmutated (UM) status (p<0.0001) and unfavorable cytogenetic lesions [del(17)(p13) and del(11)(q23)] (p<0.0001). Stereotyped HCDR3 sequences were identified in 173 of 585 patients (29.6%) and were similarly represented among patients developing AIHA (28,7%) or not (29.6%). Of the stereotyped subsets, subset #3 was associated with a significantly higher risk of AIHA occurrence than the other HCDR3 configurations (p=0.004). Restricting the analysis to UM patients, a strong association was found between AIHA and “truly” UM patients, defined as patients carrying a 100% identity with the germ line configuration. Multivariate analysis showed that “truly” UM IGHV, del(17)(p13) and del(11)(q23) were the strongest independent variables associated with risk of developing AIHA (p=0.02, p=0.0002 and p=0.01, respectively).
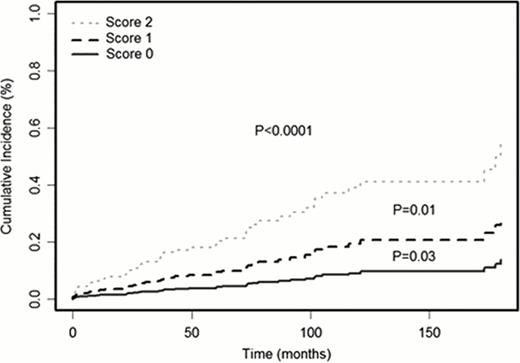
Based on the results of the multivariate analysis, we constructed a risk score of developing AIHA during time, according to the presence of none (low risk = favorable cytogenetics and mutated (M) IGHV), one (intermediated risk = unfavorable cytogenetic or UM), or two (high risk = unfavorable cytogenetic and UM) risk factors. This scoring system allowed a significant patient risk stratification (Figure 1).
Taken together, our data indicate that an UM IGHV status and/or unfavorable cytogenetic lesions are associated with the risk of developing secondary AIHA in CLL patients and suggest a possible role of specific stereotyped BCR subsets in a proportion of cases.
Prognostic score to test the risk of AIHA development over time. Patients were divided into low risk (not unfavorable cytogenetics and M IGHV), intermediate risk (unfavorable cytogenetics or UM IGHV) and high risk (unfavorable cytogenetics and UM IGHV).
Prognostic score to test the risk of AIHA development over time. Patients were divided into low risk (not unfavorable cytogenetics and M IGHV), intermediate risk (unfavorable cytogenetics or UM IGHV) and high risk (unfavorable cytogenetics and UM IGHV).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal