Abstract
Abstract 1577
Except for minor subtypes of disease with prolonged clinical courses, peripheral T cell lymphoma (PTCL) is clinically aggressive and associated with poor survival. Although the International Prognostic Index (IPI) and the PTCL prognostic index (PIT) are used for prognostic stratification, their predictive utility is in need of improvement. PTCL can be subdivided into two types, nodal and extra-nodal, the latter of which is composed of diseases with characteristic clinical presentations. The nodal group includes PTCL not otherwise specified (NOS), angioimmunoblastic T cell lymphoma (AITL), anaplastic large cell lymphoma (ALCL), and adult T cell leukemia (ATL). While ATL is a distinct disease caused by HTLV-I, the remaining three diseases have several characteristics in common, and their differential diagnosis is sometimes difficult.
Patients who were newly diagnosed with biopsy-proven, HTLV-I-negative nodal PTCL and referred to our institution between May 1994 and February 2012 were retrospectively analyzed. Patients treated with regimens not intended to induce remission, as well as those with insufficient clinical data, were excluded. This study was Institutional Review Board-approved and complied with the Declaration of Helsinki. The diagnoses were primarily based on histopathology, and in select instances, molecular and immunological analysis was used to support the diagnosis. The overall survival rate (OS) and progression-free survival rate (PFS) were calculated using the Kaplan-Meier method and significance was determined by log-rank test. Univariate and multivariate analyses were performed with the Cox proportional hazards regression model.
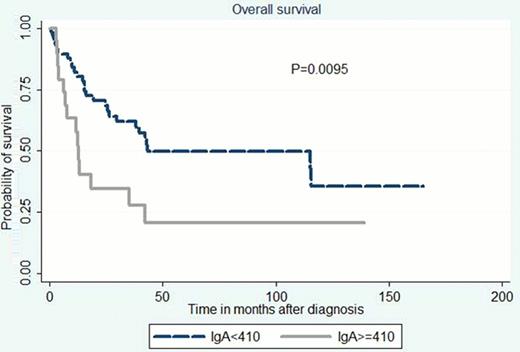
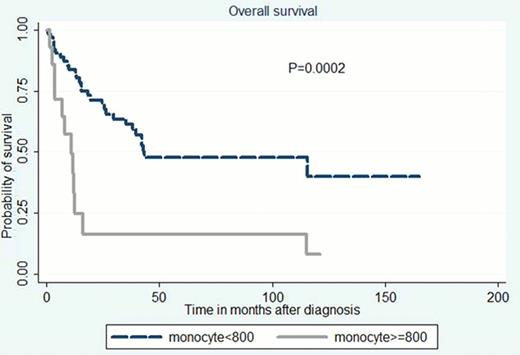
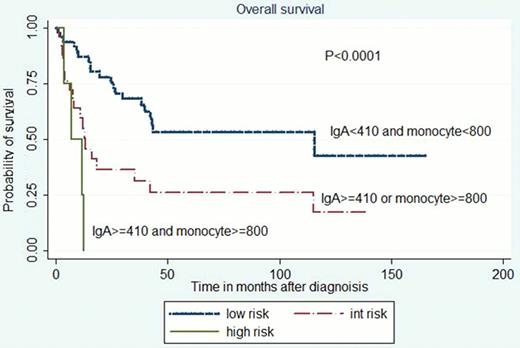
A total of 77 patients, including 50 PTCL-NOS, 17 AITL, and 10 ALCL patients, 5 of whom were ALK-positive, were identified. The median follow-up time for survivors was 49 months. The median age was 65 years (range, 23–83), and there was a male predominance (male/female ratio: 1.95). 61 had advanced stage (stage III/IV), 20 had more than 1 site of extranodal involvement, and 20 had documented bone marrow involvement. 35 had ECOG performance status of greater than 1. Laboratory data showed elevated serum LDH level in 55. The IPI score was greater than 2 in 47, and the PIT score was greater than 1 in 50. All but one were treated with anthracycline-containing combination chemotherapies. In addition, 16 received high-dose chemotherapy with autologous stem cell rescue. The 5 year OS for the entire population was 42%, and histological diagnosis did not significantly affect OS (the OS for PTCL-NOS, ALCL, and AITL was 35%, 67%, and 47%, respectively). To explore prognostic factors further, univariate analysis was performed using various pretreatment characteristics. Variables significantly associated with poor survival were advanced stage, extranodal involvement > 1 site, bone marrow involvement, anemia, monocyte ≥800 /μL, soluble interleukin-2 receptor > 3,000 U/mL, serum IgG ≥1700 mg/dL, and serum IgA ≥410 mg/dL. The IPI classification was highly correlated with prognosis in this cohort: the relative risk of death was 2.78, 3.99, and 5.61 times higher for pts with IPI of LI, HI, and H, respectively, when compared with IPI L pts (log-rank test; P = 0.0213). By contrast, the PIT classification did not have prognostic value. Then, by using variables associated with poor survival by univariate analysis and not included into IPI, prognostic variables independent of IPI were identified on multivariate analysis. Monocytosis and elevated serum IgA levels were significantly associated with poor survival independently of IPI. The dichotomized monocyte and IgA were combined to generate an IgA/monocytosis prognostic score and pts were stratified into three risk groups: low (IgA < 410 mg/dL and monocyte < 800 /μL), int. (IgA ≥410 or monocyte ≥800), and high-risk (IgA ≥410 and monocyte ≥800) populations. The relative risk of death was 8.56 and 2.83 times higher for pts in the high and int. risk groups, respectively, when compared to the low-risk population (P < 0.0001). Clearly, the new prognostic score was able to stratify pts by risk in a manner comparable to the IPI.
Monocytosis and high IgA levels were a novel prognostic factor independent of IPI in the limited number of HTLV-I-negative nodal PTCL patients included in this retrospective study. Further analysis is warranted in a greater number of patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal