Abstract
Abstract 1525
Nodular lymphocyte predominant Hodgkin Lymphoma (NLPHL) is a more indolent form of Hodgkin Lymphoma that is usually associated with favorable outcomes. However, a number of reports have shown a tendency of transformation to more aggressive types of lymphoma, typically diffuse large B-cell lymphoma (DLBCL). Long-term data on the incidence and outcomes of transformed NLPHL is lacking in the literature. The aim of this study was to evaluate incidence, risk factors and outcomes of DLBCL transformation in NLPHL in a cohort of patients followed at a single institution.
The actively maintained Mayo Clinic Lymphoma Database includes all consenting consecutive patients with lymphoma seen at Mayo Clinic Rochester. This was used to retrospectively identify patients with NLPHL. The study was approved by the Institutional Review Board. Pathology was reviewed by a hematopathologist and all transformations were histologically confirmed by WHO criteria. The clinical characteristics, therapy and outcomes of patients with NLPHL and DLBCL transformation were analyzed. The chi-square test was used to compare variables. Risk of progression was calculated using a person-year approach. Survival and freedom from transformation were estimated and compared using the Kaplan Meier method and log rank tests, respectively.
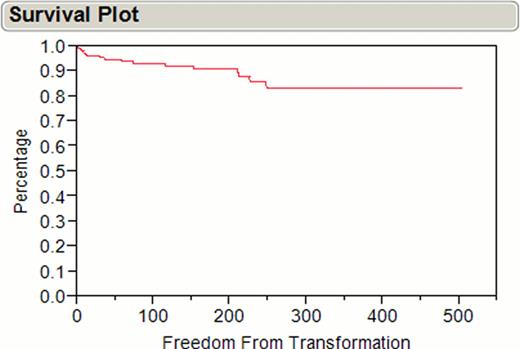
Between 1970 and 2010, 222 consecutive adult patients with NLPHL were identified. The median follow-up was 20 years. Of these, 17 (7.7%) developed a transformation to DLBCL during the course of the disease (Figure 1). The median time to transformation was 35 (6–248) months. Of these 17 patients, 13 (76.5%) were male, 11 (64.7%) had stage I/II and 6 (35.3%) had stage III/IV NLPHL. Transformation was the first relapse in most patients (12 patients, 70.6%) while five patients (29.4%) developed one or more relapses of NLPHL before transformation. Prior therapies for NLPHL were as follows: radiation therapy in 5 (29.4%), chemotherapy in 5 (29.4%) and combined chemotherapy and radiation in 6 (35.3%) patients. The median age at transformation was 45 years (30–87). Most patients (10 patients, 58.8%) presented with signs (palpable lymph nodes) or “B” symptoms. Eight patients (47.1%) had stage III/IV disease at the time of transformation. The most commonly used regimens for treatment of DLBCL were R-CHOP or CHOP (9 patients, 52.9%). Platinum based therapy was administered in 4 (23.5%) patients. Five patients (29.4%) required more than one line of therapy, and autologous stem cell transplant was utilized in two (11.7%) patients.
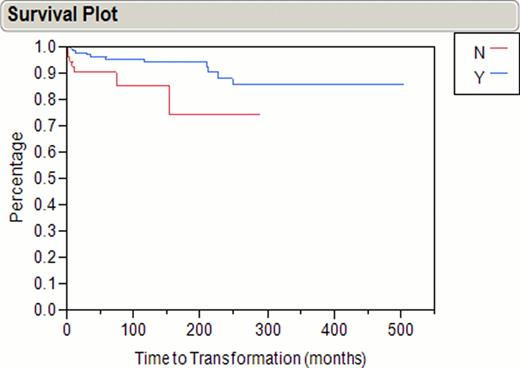
Based on the observed 17 transformations during 2304 patient-years of follow-up, the rate of transformation was 0.74 per 100 patient-years. The five-year overall survival (OS) of patients with transformed disease (calculated from time of transformation) was 76.4%. The most common cause of death was lymphoma (75%). Following treatment for transformation, 5 patients (29.4%) relapsed. The OS in transformed patients was independent of prior therapies, and transformation did not adversely affect overall survival in our cohort (median survival of in 129 months in transformed versus 120 in non-transformed patients, P=0.33). In a univariate analysis of prior therapies, use of radiation therapy was associated with a significant delay in time to transformation (P= 0.0035) (Table 1, figure 2).
The risk of transformation in NLPHL is 0.74% per year in this large single institution case series of NLPHL, and appears to be lower than that observed in follicular and other types of low grade lymphoma. The outcomes of patients with transformation were significantly better than reported in other types of transformed lymphoma and did not adversely affect OS.
Univariate Analysis of Prior Therapies Correlated with Freedom from Transformation in NLPHL (222 patients)
| Prior therapy . | P-value . |
|---|---|
| Prior RT | 0.0035 |
| Any chemotherapy | 0.7 |
| ABVD | 0.1 |
| CHOP | 0.2 |
| MOPP | 0.2 |
| Platinum-based chemotherapy | 0.5 |
| Rituximab based chemotherapy | 0.6 |
| ASCT | 0.7 |
| Prior therapy . | P-value . |
|---|---|
| Prior RT | 0.0035 |
| Any chemotherapy | 0.7 |
| ABVD | 0.1 |
| CHOP | 0.2 |
| MOPP | 0.2 |
| Platinum-based chemotherapy | 0.5 |
| Rituximab based chemotherapy | 0.6 |
| ASCT | 0.7 |
RT= radiation therapy, NLPHL=nodular lymphocytic predominant Hodgkin lymphoma, ABVD=Doxorubicin, Bleomycin, Vinblastine, and Dacarbazine. CHOP= Cyclophosphamide, Vincristine, Doxorubicin, and Prednisone, ASCT=autologous stem cell transplantation.
Freedom from Transformation with the Use of Prior Radiation Therapy in NLPHL (222 patients)
Freedom from Transformation with the Use of Prior Radiation Therapy in NLPHL (222 patients)
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal