Abstract
Abstract 1096
ITP is an autoimmune disorder characterized by increased platelet destruction and/or decreased platelet production. In addition to risks of bleeding, an increased risk of thrombosis has been identified, despite low platelet counts. Reasons behind this remain unclear. Elevated levels of VWF and decreased levels of ADAMTS13 have been observed in patients with myocardial infarction and ischaemic stroke. Given the interaction of these plasma proteins with platelets, we hypothesized that changes in VWF/ADAMTS13 levels may contribute to the thrombotic risk in patients with ITP.
Adult patients (>18 years) with a diagnosis of ITP were included. ELISAs were used to measure the concentrations of VWF, ADAMTS13 and IL-6. Platelet count and C-Reactive protein (CRP) levels were recorded. Control samples for VWF and ADAMTS13 were taken from a previous study (n=626) (Andersson et al. Blood 2012; 119(6):1555–60). Published data from a population-based study (Marques-Vidal et al. PLoS One 2011; 6(6): e21002) enabled comparison of IL-6 levels to normal controls.
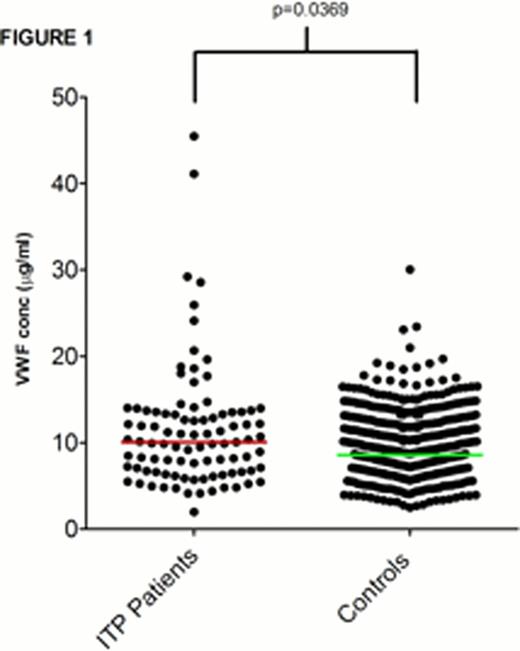
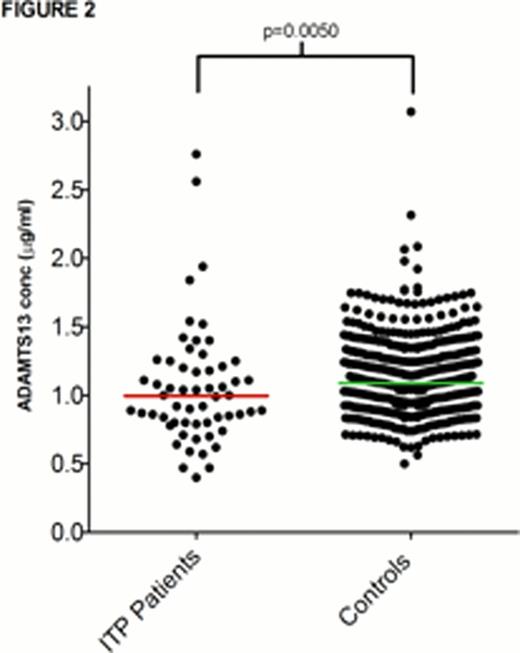
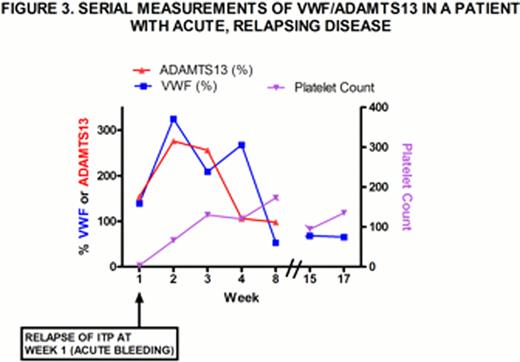
93 samples were taken from 48 patients with ITP between March-June 2012. All samples were analyzed for VWF:Ag levels. Plasma concentrations of ADAMTS13 and IL-6 were analyzed in 58 and 34 plasma samples respectively. Plasma VWF antigen (VWF:Ag) levels were elevated in patients with ITP compared to control subjects (p=0.0369) (Figure 1). Levels of ADAMTS13 in patients with ITP were lower than those for control subjects (p=0.0050) (Figure 2). Plasma VWF levels did not correlate with platelet counts. Rather high VWF levels were specific to certain patients. Two patients with VWF:Ag levels >40 μg/mL had a past history of thrombosis; both had additional co-morbidities. Two further patients with acute disease (one recent acute intracranial bleed and one new relapse of ITP) also had high VWF levels. In these two patients, VWF, ADAMTS13 and platelets change over time (example shown in Figure 3). CRP levels did not correlate with platelet count (p=0.6091) or with VWF:Ag levels (p=0.5170). Median IL-6 levels were raised in patients with ITP (3.785 pg/mL) compared to healthy controls (1.47 pg/ml) (p=<0.0001). IL-6 correlated positively with CRP levels (p=0.0183, r=0.4211) however no association between IL-6 and VWF, ADAMTS13 or platelet count was established.
The increased ratio of VWF: ADAMTS13 may be contributory in the pathogenesis of thrombosis, in particular in patients with acute and unstable disease. Increased VWF:ADAMTS13 ratio may also result in an increased VWF activity, even without a rise in total VWF. Future studies comparing VWF:Ag to collagen binding are planned.
The mechanism behind fluctuating levels of VWF and ADAMTS13 remains unclear. We investigated whether inflammatory mediators associated with acute disease could play a role. CRP levels were elevated in many patients with ITP, but this did not correlate with VWF levels. Levels of IL-6 were also significantly raised in patients compared to healthy controls and correlated with CRP but did not correlate with VWF or with platelet count.
In summary, ITP appears to be a heterogeneous disease. In some patients, autoimmunity may be associated with an inflammatory process, and in other patients, low platelets may interfere with other aspects of the coagulation system. Either may predispose to thrombosis or bleeding. Further investigation of the interactions of platelets, with inflammatory cytokines and the coagulation system may help us to better understand the disease, and to recognize those patients at risk of bleeding, or conversely thrombosis.
Cooper:Amgen: Consultancy; GSK: Consultancy; Easai: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal