Abstract
Abstract 1040
Hemophagocytic syndrome (HPS) is a rare disorder characterized by fever, splenomegaly, cytopenias, hypofibrinogenemia, hyperferritinemia and hemophagocytosis in the bone marrow or lymph nodes. It is caused by pathologic activation of the immune system, and manifests clinically with signs and symptoms related to extreme inflammation. Primary HPS or familial hemophagocytic lymphohistiocytosis (HLH) occurs predominantly in children (<18 years) due to inherited defects in natural killer and cytotoxic T-cell function. Secondary HPS generally occurs in adults (>18 years) and is precipitated by autoimmune disorders, malignancy and a variety of infections. The results of HLH-94 trial, the largest prospective study in pediatric patients with HLH, reported an estimated 5-year survival of 54%. There is a paucity of information about HPS in adult patients.
Records of all adult (≥ 18 years) patients with a diagnosis of “hemophagocytosis“ or “hemophagocytic syndrome” presenting from January 1996 through December 2011 at Mayo Clinic were reviewed. Our hematopathology database was also analyzed for patients bearing a diagnosis of HPS. Out of a total of 127 patients identified in the database, 50 adult patients were diagnosed to have HPS as per the diagnostic criteria of the HLH-1994 trial (for patients seen prior to 2004), and HLH-2004 trial (for patients seen after 2004). This study was approved by the Institutional Review Board at Mayo Clinic.
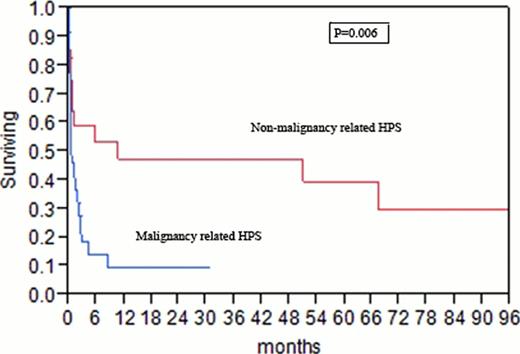
Baseline characteristics of all patients are shown in Table 1. The median time to diagnosis from the onset of symptoms was 38 days (4–158 days). Secondary HPS was diagnosed in 46 (92%) patients. The causes of secondary HPS are shown in Table 2. Twenty (40%) patients were treated with etoposide containing regimen, 26 (52%) were treated with therapeutic agents directed specifically to the underlying precipitating disease, and 4 (8%) patients did not receive any treatment. No patient in our study underwent a stem cell transplant (SCT). After a median follow-up of 43 months, 36 (72%) patients have died. The causes of death were infection (47%), malignancy (42%), bleeding (8%) and unknown (3%). The median overall survival (OS) for the entire cohort was 1.5 months (95% CI, 0.7–4.5 months). The median OS for patients with malignancy- related HPS was 0.8 months (95% CI, 0.4–2.4 months) compared to 11 months (95% CI, 0.7-not reached) for patients with non-malignancy related HPS (p-value:0.006; Figure). On univariableanalysis, factors associated with a worse survival were serum albumin <2 g/dL (hazard ratio, 8.3), malignancy-related HPS (hazard ratio, 7.3) and serum creatinine >1.3 mg/dL (hazard ratio, 3.8).
In this large series of adult HPS patients treated at a single tertiary care center, most cases are secondary, and are associated with a worse survival compared to historical outcomes reported for children enrolled on the HLH-94 trial. This is likely related to a marked delay in referral to our institution, and high early mortality precluding consideration of SCT. Adult patients with malignancy- related HPS in this study had a markedly inferior outcome compared to patients with non-malignancy related HPS.
| Characteristic . | (Range) or [%] . | |
|---|---|---|
| Total Number of patients | 50 | |
| Median Age, years | 49 (18–87) | |
| Males | 33 [66] | |
| Median hemoglobin, gm/dL | 9 (6.2–13.7) | |
| Median total WBC (x109/L) | 1.8 (0.2–43.5) | |
| Median absolute neutrophil (x109/L) | 1.2 (0–33.6) | |
| Median platelet (x109/L) | 55 (6–288) | |
| Median aspartate aminotransferase (U/L) | 111 (10–9450) | |
| Median total bilirubin (mg/dL) | 1.9 (0.3–25.6) | |
| Median lactate dehydrogenase (U/L) | 472 (90–9290) | |
| Serum triglycerides (mg/dL) | Median | 252 (68–831) |
| >265 | 14 [28] | |
| <265 | 20 [40] | |
| Not available | 16 [32] | |
| Serum fibrinogen (mg/dL) | Median | 160 (50–585) |
| <150 | 22 [44] | |
| >150 | 22 [44] | |
| Not available | 6 [12] | |
| Serum ferritin (ng/mL) | Median | 8400 (372–140,690) |
| <500 | 1 [2] | |
| 501–3000 | 16 [32] | |
| >3001 | 24 [48] | |
| Not available | 9 [18] | |
| Characteristic . | (Range) or [%] . | |
|---|---|---|
| Total Number of patients | 50 | |
| Median Age, years | 49 (18–87) | |
| Males | 33 [66] | |
| Median hemoglobin, gm/dL | 9 (6.2–13.7) | |
| Median total WBC (x109/L) | 1.8 (0.2–43.5) | |
| Median absolute neutrophil (x109/L) | 1.2 (0–33.6) | |
| Median platelet (x109/L) | 55 (6–288) | |
| Median aspartate aminotransferase (U/L) | 111 (10–9450) | |
| Median total bilirubin (mg/dL) | 1.9 (0.3–25.6) | |
| Median lactate dehydrogenase (U/L) | 472 (90–9290) | |
| Serum triglycerides (mg/dL) | Median | 252 (68–831) |
| >265 | 14 [28] | |
| <265 | 20 [40] | |
| Not available | 16 [32] | |
| Serum fibrinogen (mg/dL) | Median | 160 (50–585) |
| <150 | 22 [44] | |
| >150 | 22 [44] | |
| Not available | 6 [12] | |
| Serum ferritin (ng/mL) | Median | 8400 (372–140,690) |
| <500 | 1 [2] | |
| 501–3000 | 16 [32] | |
| >3001 | 24 [48] | |
| Not available | 9 [18] | |
| Etiology of Secondary HPS . | Total Number of Patients = 46 (%) . | |
|---|---|---|
| Malignancy | Total | 23 (46) |
| T-cell lymphoma | 14 | |
| B-cell lymphoma | 5 | |
| Hodgkin's lymphoma | 1 | |
| Myeloid neoplasm | 1 | |
| Solid organ | 1 | |
| Other (systemic histiocytosis) | 1 | |
| Infection | Total | 19 (38) |
| Ebstein Barr virus | 7 | |
| Cytomegalovirus | 3 | |
| Nonspecific viral infection | 3 | |
| Histoplasmosis | 3 | |
| Bacterial | 2 | |
| Blastomycosis | 1 | |
| Autoimmune | Total | 4 (8) |
| Etiology of Secondary HPS . | Total Number of Patients = 46 (%) . | |
|---|---|---|
| Malignancy | Total | 23 (46) |
| T-cell lymphoma | 14 | |
| B-cell lymphoma | 5 | |
| Hodgkin's lymphoma | 1 | |
| Myeloid neoplasm | 1 | |
| Solid organ | 1 | |
| Other (systemic histiocytosis) | 1 | |
| Infection | Total | 19 (38) |
| Ebstein Barr virus | 7 | |
| Cytomegalovirus | 3 | |
| Nonspecific viral infection | 3 | |
| Histoplasmosis | 3 | |
| Bacterial | 2 | |
| Blastomycosis | 1 | |
| Autoimmune | Total | 4 (8) |
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal