Abstract
Aging and the physiologic decline of tissues and cells were once thought to be irreversible. However, recent studies suggest that various tissues, especially parts of the hematopoietic system, can be rejuvenated. Here we review potential mechanisms for this process and how they may be used to reverse age-related disorders and aging in general. We propose the novel hypothesis that altering the homeostatic process during cellular depletion can reverse aging in the hematopoietic system.
Effect of age on tissue formation and function
Physiologic aging initiates from the onset of reproductive maturity and generally affects almost every aspect of the organism. In the process of aging, homeostatic mechanisms controlling tissue formation and function are gradually changing, resulting in reduced fertility, tissue dysfunction, and increased susceptibility to diseases. All these changes impact the quality of life and stimulate extensive research to unravel the biologic mechanisms of aging and to develop novel approaches to inhibit or to reverse age-related disorders.
Despite the increase in life expectancy during the last century,1,2 this extension of life is not supported by the body's physiologic systems, which nonetheless continue to “age.” The failure of these systems and/or their adaptation to the extended survival is reflected by the increased incidence of age-related disorders.
Homeostasis in tissues reflects equilibrium between generation and differentiation of new cells on the one hand and death of cells on the other hand. Throughout life, this homeostasis ensures growth, maintenance, and healthy function of the different physiologic systems in the body. However, the roles of homeostasis are different for tissues with regenerative capacities, such as epithelial tissue and blood, relative to tissues without regenerative capacity, such as muscle and nerve.3-8 In the absence of a regenerative capacity, attempts are now being made to inhibit the age-related cell loss and to apply tissue engineering technologies to repair permanent muscle and nerve tissue damages to reduce heart disease and neurodegenerative disorders.
Tissues with a regenerative capacity constantly produce new cells throughout life. This is facilitated by the presence of proliferating and differentiating tissue-specific stem cells. Nevertheless, these tissues are not devoid of age-related alterations. For example, despite accumulation of senescent characteristics in the aged skin, epidermal stem cells are maintained at normal levels throughout life. Skin aging in this case may be induced by impaired stem cell mobilization or their reduced response to proliferative signals.9 Similarly, in the gut epithelium and liver, the capacity of cellular renewal throughout life by tissue stem cells may be affected by lower sensitivity to growth factors and activation of cell cycle and mitogenic gene.10,11 Thus, tissues with a regenerative capacity change with aging, but their regenerative capacity is not abolished, a theme we revisit herein.
Aging in the hematopoietic system
Hematopoietic stem cells (HSCs) give rise to all blood cells through proliferation, lineage commitment and differentiation. Early pluripotent stem cell in the BM give rise to stem cells of more limited developmental potential, which are the early progenitors of red blood cells, platelets, and the main categories of white blood cells, the lymphoid and myeloid lineages. It is now known that there are several HSC subpopulations differing in their differentiation programs and lineage commitments. The size of each HSC subpopulation as well as their self-renewal and differentiation behaviors are regulated by intrinsic and extrinsic mechanisms.12,13 Changes in HSC populations develop with age, which alter cellular composition, lineage commitment, and their proliferative capacity.12,13 However, despite these changes, production of red blood cells, platelets, and the myeloid lineage cells does not significantly change with age. This production overcomes the constant loss of these cells, which are relatively short lived and have no self-renewal capacity. Thus, cellular homeostasis regulates cell production in the hematopoietic system and fits well within the concept in which early cell lineages adapt their output to demand.14,15 With age, though, abnormalities in these lineages, such as myeoloproliferative diseases and a greater propensity for anemia, do occur.16,17
In contrast, the lymphoid lineage is dramatically altered in aging and production of lymphocytes is essentially diminished in the aged BM.12,13 Studies with HSCs revealed that the majority of HSCs from elderly mice are myeloid biased, whereas most HSC from young mice are balanced in lymphopoiesis and myelopoiesis,18,19 explaining the increase in myelopoiesis with aging.20-22 Several reasons may account for the reduced production of lymphocytes (see below), but unlike cells of other lineages, lymphocytes, especially antigen-experienced memory cells, are relatively long-lived with some homeostatic proliferation capacities.23-25 Thus, despite the diminished production in the BM and the involution of the thymus, the absolute numbers of T and B lymphocytes in the peripheral organs does not significantly change with aging.26-29 However, the response of these long-lived cells to new antigenic challenge is poor in quality and quantity. Consequentially, this renders the elderly more susceptible to infectious diseases and poorly responsive to vaccination.30-33
Why lymphopoiesis declines with aging?
Lymphocytes develop from early common lymphoid progenitors, which differentiate into T and B lineage cells. During their development, lymphocytes rearrange and assemble antigen receptor genes to express specific receptors. Developmental progression is guided by the successive gene recombination and is supported by trophic soluble factors and receptor-ligand interactions.34-36 Positive and negative selection events ensure the construction of a safe and functional peripheral compartment, which constitutes the maximal breadth of antigen receptor diversity that is capable to recognize any given antigen.37-40 In the adult, the size of this compartment is maintained by equal production and loss rates.41
However, the rate of lymphopoiesis dramatically declines with aging because of intrinsic and extrinsic factors affecting hematopoietic stem cells, as well as early and late lymphoid progenitors. Studies have shown that the lineage potential of long-term HSCs changes with age, whereas lymphoid differentiation diminishes in favor of myeloid differentiation.20-22 A genome-wide expression profile of aging stem cells revealed altered gene expression and accumulation of DNA damage that affects multiple signaling pathways and cell cycle regulation.21,42,43 This DNA damage may alter lineage potential and responsiveness to trophic signals, as has been proposed.20,44 Indeed, it has been demonstrated that the composition of the stem cell compartment in aging is dominated by myeloid-biased HSCs,18,19,45 with down-regulation of genes directing lymphoid lineage and up-regulation of genes directing myeloid lineage.20,21,46 The outcome of these alterations is the significant reduction in the frequencies of common lymphoid progenitors21,47-50 and, consequentially, a diminished lymphopoiesis. Further, a recent study identified a developmental checkpoint that limits stem cell self-renewal in response to DNA damage by promoting their differentiation. Using RNAi screens, a basic leucine zipper transcription factor ATF-like has been identified as a major component that is up-regulated primarily in lymphoid-biased HSCs in response to the accumulation of DNA damage and subverts their self-renewal capacity.51 This study now provides an important mechanistic explanation for the selective loss of lymphoid potential in aging.
Production of T lymphocytes depends on further development and selection of progenitor cells in the thymus, which undergoes atrophy with age. Thymic involution is one of the major features of immunosenescence and is characterized by a progressive reduction in size because of changes in its anatomic structure, including reduction in areas of thymopoiesis and accumulation of fat.52,53 The progressive involution of the thymus eventually abolishes the output of naive T cells in aging, and any attempt to reverse T-cell aging should include the restoration of functional thymic tissue. Several hormones, sex steroids, growth factors, and cytokines have been shown to inhibit or partially restore thymic tissue.54 The plasticity of the thymic tissue also has been shown in a recent study where the cortical thymic epithelial cell compartment had regenerated after conditional ablation and restored T-cell development.55
B lymphocytes primarily develop in the BM. In adult mice, 1-2 × 107 immature B cells are generated daily and only ∼ 3% survive positive and negative selection to enter the pool of mature B cells, mainly into the follicular compartment.56 Naive follicular B cells are short-lived (40-120 days) and are constantly replenished by new B cells produced in the BM.57 In aging, the generation of immature B cells in the BM declines.49 In addition to the age-related changes in HSCs, other factors have been shown to contribute to the loss of B lymphopoiesis. These include a reduction of B-cell progenitor frequencies49 and in their proliferative potential,58 decreased IL-7 production,59 and impaired V-DJ rearrangement.60 The latter appears not to result from altered expression of recombination-activating genes but from changes in the expression of the E2A-encoded, E12 and E47 basic helix-loop-helix proteins that bind the IgH promoter.61 Several in vivo experimental approaches have demonstrated the poor B lymphopoiesis in the aging BM. When BM cells or purified HSCs from old donors were adoptively transferred into irradiated recipient mice, they poorly reconstituted the peripheral B-cell compartment.21,62-64 Taken together, the observations supported the argument that age-related decline in B lymphopoiesis is a progressive and irreversible process. But this does not appear to be the case as detailed in the next section.
Another intrinsic mechanism that may contribute to the altered B lymphopoiesis in aging is the properties of pre-BCR expression and signaling and the consequential effects on B1 versus B2 cell development. A study by Alter-Wolf et al has shown that, whereas B2 cell development diminishes with aging, B1 cell development remains unaltered.65 In this study, they propose that, with aging, expression level of surrogate light chain in B2 progenitors decreases and becomes not different from that in B1 progenitors, thus generating a larger pool of B cells with B-1 like properties in the old BM. This mechanism, however, does not explain the altered composition and the decline in lymphoid commitment of the HSC populations.12,13
Age-related changes of the lymphoid lineage in the periphery
Despite the decline in lymphopoiesis, there are no significant changes in the absolute numbers of peripheral B and T lymphocytes with aging.26,28 However, the cellular composition of the peripheral compartment is dramatically changed in old age. Perhaps the most significant change is the accumulation of long-lived memory cells and the decline in frequencies of naive cells. Kline et al have used kinetic labeling experiments and demonstrated that peripheral B cells in aged mice have a much longer life span than peripheral B cells in young mice.27 Indeed, analysis of B-lineage cells in old mice revealed a significant decrease in the number of naive B-2 cells, which are short-lived and primarily reside in the follicular compartment, and a significant increase in peripheral B cells expressing antigen-experienced long-lived phenotypes, including memory B cells, B-1 cells, and marginal zone B cells.26,66 The decline of follicular B cells results in a significant reduction in the B-cell repertoire because follicular B cells express unmutated antigen receptors and exhibit the most diverse specificities. This has been confirmed by spectrotype analyses and was found to correlate with poor health status67,68 and with poor responsiveness to vaccination.69,70 Importantly, this poor responsiveness is most pronounced in terms of those to new or evolving pathogens, whereas responsiveness to recall by the memory compartment increases with age.71 In addition, several intrinsic defects have also been shown to contribute to the poor B-cell responsiveness in aging. Thus, expression of activation-induced cytidine deaminase and consequential class switch recombination is altered in B cells from aged persons, possibly because of decreased expression of E2A-encoded transcription factor E47 on stimulation.72 Retrovirally driven overexpression of E47 was able to rescue these intrinsic defects.73
Recently, a novel B-cell subset has been shown to accumulate in the periphery with aging named aging-associated B cells.74,75 These cells respond to innate stimulation (Toll-like receptor 7 and Toll-like receptor 9) but are refractory to BCR-driven activation and are independent of BLyS for survival. Aging-associated B cells are thought to be generated from mature B cells that expand during immune responsiveness throughout life and compete with naive follicular B cells for niche space and for the trophic homeostatic cytokine BLyS.75
Consequent to the decrease in thymopoiesis with aging, there is a decline in naive CD4+ and CD8+ T cells in both diversity and functional integrity, resulting in poor responsiveness to vaccination.29,33 In parallel, the number of antigen-experienced memory and effector cells increases with age. Furthermore, naive T cells from aged persons exhibit numerous functional defects, including shorter telomeres, reduced cytokine production, and impaired expansion and differentiation into effector cells after antigen stimulation.76 Collectively, the age-related changes in the peripheral B and T lymphocyte compartments constitute the primary cause for immune incompetence in aging.
Is aging in the B lineage a reversible process? A possible model
Approaches for reversible aging in the adaptive immune system should focus at the level of cell development rather than attempting to apply changes in end-stage differentiated cells. To this end, attempts to rejuvenate the B lineage must be targeted to the hematopoietic system to reactivate the B-cell production in the BM and to increase the flow of naive B cells to the peripheral compartment. However, as detailed under “Aging in the hematopoietic system,” there are several studies showing that HSCs acquire defects affecting their proliferative capacity and their commitment to the lymphoid lineage. This is thought to lead to a progressive and irreversible decline in B lymphopoiesis. Indeed, total BM cells or purified HSCs from old donors that were adoptively transferred into irradiated recipient mice poorly reconstituted the peripheral B-cell compartment.21,62-64 Similarly, lymphoablation in old mice by cyclophosphamide or irradiation induced poor autoreconstitution of the peripheral B-cell compartment compared with that of young controls.77 In one of these studies, Guerrettaz et al used an immunoglobulin transgenic mouse to show that this poor regenerative capacity contributes to the generation of altered B-cell repertoire in the periphery.62
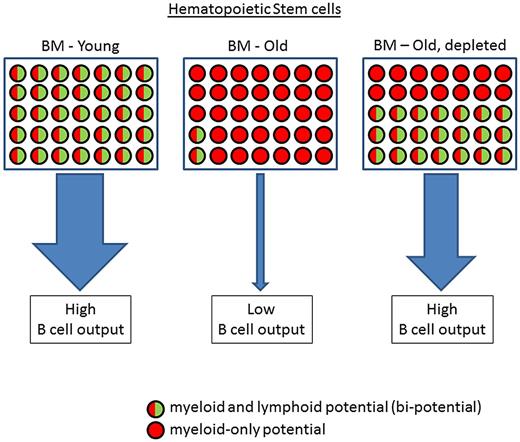
However, although the study by Guerrettaz et al62 apparently favors the irreversible model, there is another interpretation for these observations. This explanation relies on homeostatic regulation and the well-described feedback mechanisms operating in other hematopoietic lineages, such as red blood cells and myeloid cells, which remain minimally affected in aging. Accordingly, as shown in Figure 1, the HSC compartment is composed from bipotential cells that can differentiate to the myeloid and lymphoid lineages. The size of this bipotential compartment is determined by homeostatic processes encompassing the peripheral need for production of new B lymphocytes to repopulate in the periphery. In young mice, where most of the B cells in the periphery are naive follicular, the frequency of the bipotential HSCs in the BM is high to ensure high output of B cells from the BM to the periphery to replenish the constant loss of naive B cells because of selection processes and their relatively short half-life. With age, long-lived memory B cells accumulate in the periphery, thus reducing the need for B-cell production in the BM.
Proposed model for changes in the cellular composition of the HSC compartment with aging. In young mice (left), the frequency of bipotential HSCs is high and thus supports high output of B cells from the BM. With aging (middle), long-lived memory B cells accumulate in the periphery, thus reducing the “need” for production of new B cells. To facilitate this, the HSC composition changes and is dominated by myeloid-only potential HSCs, leaving only a small number of bipotential HSCs. With depletion of the long-lived B cells (right), the peripheral “need” for B cells stimulates expansion of the bipotential HSCs to reactivate B lymphopoiesis in the aged BM and revives the flow of new B cells from the BM to the periphery.
Proposed model for changes in the cellular composition of the HSC compartment with aging. In young mice (left), the frequency of bipotential HSCs is high and thus supports high output of B cells from the BM. With aging (middle), long-lived memory B cells accumulate in the periphery, thus reducing the “need” for production of new B cells. To facilitate this, the HSC composition changes and is dominated by myeloid-only potential HSCs, leaving only a small number of bipotential HSCs. With depletion of the long-lived B cells (right), the peripheral “need” for B cells stimulates expansion of the bipotential HSCs to reactivate B lymphopoiesis in the aged BM and revives the flow of new B cells from the BM to the periphery.
As an adaptation, cellular homeostasis may gradually change the HSC composition in the old BM to increase the fraction of cells bearing myeloid-only potential (which are continuously produced throughout life) and to decrease the fraction of the bipotential HSCs. This may occur by selection and/or preferential expansion of HSC populations that have altered gene expression to favor myeloid lineage differentiation. Indeed, such altered gene expression profiles have been found in HSCs from old mice.20,21,42,43 Most importantly, as shown in Figure 1, although the frequency of the bipotential HSCs drops with aging because of homeostatic pressures, it is never completely abolished. This explains why some B lymphopoiesis continues, even in old age. There are 2 main studies that support this change in the cellular composition of the HSC compartment: (1) it has been shown that aging is associated with changes in the clonal composition of the HSC compartment and is dominated by myeloid-biased HSCs18,19,45 ; and (2) a subpopulation of HSCs (expressing Slamf1low) retaining an equivalent potential to differentiate into lymphoid and myeloid lineages has recently been identified with significantly reduced frequencies in aging mice.18 Hence, in the study by Guerrettaz et al,62 the failure of the HSCs from old mice to reconstitute the B lineage may simply reflect the small amount of bipotential HSCs within the transferred cells, which contained mostly cells with a myeloid-only potential. Their finding, that increasing the number of the transferred cells improves the reconstitution of the peripheral B-cell compartment by both cell number and the skewed repertoire,62 supports this argument. The altered HSC composition may also explain earlier studies showing that BM from old mice failed to reconstitute the peripheral B-cell compartment on B-cell ablation by cyclophosphamide or in BM chimeras.26,77 Taken together, it appears that the decline in B lymphopoiesis in aging can be explained by alterations of cellular homeostasis and consequential selection processes of HSC populations.
Reversing B-cell aging
The possibility that B-cell aging is indeed a consequence of homeostatic regulation suggests that B lymphopoiesis may be reactivated on alteration of this homeostasis. A central factor in achieving this would be the expansion of the bipotential HSC population in aging. According to this homeostasis model, the low number of HSCs limits the rate of B lymphopoiesis. Critical evidence for the importance of this HSC population in maintaining B-cell output in aging comes from analysis of B lymphopoiesis in mutated mouse models where the peripheral B-cell compartment is never filled.37,78-80 In these mice, continuous “demand” for B cells in the periphery prevents age-related alterations in the HSC compartment and the subsequent decline of B lymphopoiesis in the BM.47 These results imply that, under conditions of chronic demand for B cells in the periphery, HSCs do not accumulate defects with aging or that the nonmutated HSCs are preferentially selected to expand to retain high output of B lymphopoiesis, even in old age. Hence, the decline in B lymphopoiesis with aging in normal mice may not be the result of progressive accumulation of DNA damage or other intrinsic defects in HSCs. Rather, the major interpretation of these experiments is that the decrease of lymphopoiesis in aging reflects alterations in cellular composition of the HSC compartment because of homeostatic pressures. In this case, we speculate that any damage or other intrinsic defect that has been identified in aged HSCs may function indeed as a selection tool for variant HSCs with myeloid-only potential and thus reduces the size of the bipotential HSCs as an adaptation to the reduced “demand” for new B cells.
Another interpretation of these results is the existence of a cross-talk mechanism between hematopoietic progenitors in the BM and peripheral B cells, which controls B lymphopoiesis. Earlier studies to demonstrate such cross-talk have used young (2- to 3-month-old) mice and came to controversial conclusions. In these experiments, Park and Osmond81,82 and Cancro and Allman83 demonstrated homeostatic regulation, whereas Agenes et al84 suggested that B-cell production in the BM is autonomously regulated. Thus, although this controversy is not yet resolved, it is possible that such a feedback mechanism is developing in aging, where the peripheral B-cell compartment dramatically changes and long-lived memory B cells accumulate.
Supporting evidence for the existence of a soluble cross-talk mediator that regulate stem cell growth and differentiation in aging comes from parabiotic pairing experiments. A study by Conboy et al85 tested the influence of systemic factors in serum on aged skeletal muscle stem cell and hepatic progenitor cells by establishing parabiotic pairings (sharing their circulatory system) between young and old mice. It is shown in this study that exposing the aged progenitor cells to factors present in young serum restored their proliferation and regenerative capacities. In a similar experimental approach, Ruckh et al have shown rejuvenation of myelin sheath production by stem cells in the aging CNS on exposure to a youthful systemic milieu through parabiotic pairings.86 Identification of these factors would enable the rejuvenation of stem cell function in aging and the restoration of age-related alterations in different tissues.
Another approach to validate the homeostatic model for B-cell aging is to apply B-cell depletion methodology to modify B-cell homeostasis and to reactivate B lymphopoiesis in aging. Keren et al48 used 3 different experimental mouse models to deplete peripheral B cells in old mice and showed reversal of aging as indicated by: (1) increased frequency of lymphoid-biased HSCs in the BM, (2) reactivation of B lymphopoiesis, (3) replacing the peripheral B-cell compartment with cells bearing “young-like” phenotype and repertoire, and (4) enhancement of the antibody response to a new antigenic challenge.
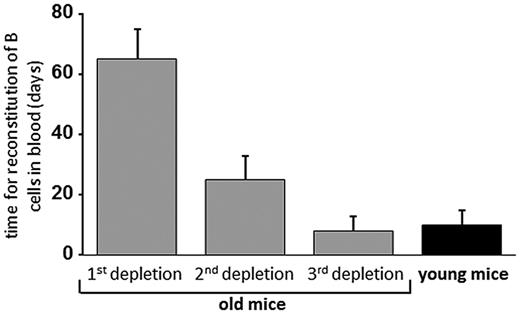
In one of these models, B-cell depletion was achieved in old mice by antibodies that were rapidly cleared from the circulation, thus enabling these researchers to follow the kinetics of B lymphopoiesis immediately after B-cell depletion is achieved. A summary of this experiment in Figure 2 clearly shows that old mice treated for one round of B-cell depletion poorly reconstituted the peripheral blood with B cells, compared with young mice (70 days relative to 10 days). This is in agreement with the results published by Guerrettaz et al showing poor B-cell reconstitution when HSCs from old mice were transferred into irradiated young recipients.62 Alternatively, we interpret their results as a reflection of low frequency of bipotential HSCs rather than incompetence of HSCs resulting from intrinsic defects. The kinetics of B-cell return after the second and the third rounds of depletion, thereby supporting our interpretation as the time to reconstitute dramatically drops to become similar to that of young mice, thus reflecting the gradual increase in the frequency of bipotential HSCs with the increasing number of B-cell depletion rounds. Analysis of the BM for B lymphopoiesis confirmed these observations.48 Hence, it appears that the HSC compartment in the aging BM still has the plasticity to adapt its cellular composition in response to homeostatic pressures and to reactivate B lymphopoiesis. Thus, the recently identified bipotential HSC population, which drops to a very low frequency in aging mice,18 may expand again in response to B-cell depletion and the homeostatic demands for B cells in the peripheral compartment (Figure 1). Yet, it is still unknown how this cross-talk mechanism operates.
Regeneration of B cells in mice after depletion. Old mice were treated for multiple rounds of B-cell depletion and were followed for the kinetics of B-cell return by analysis of peripheral blood. The second and the third depletion events were introduced only after > 80% reconstitution was achieved. Gray bars represent the average time for B-cell reconstitution after each depletion, and black bar, the time needed for B-cell reconstitution in young mice. These data summarize the experiments of Keren et al.48
Regeneration of B cells in mice after depletion. Old mice were treated for multiple rounds of B-cell depletion and were followed for the kinetics of B-cell return by analysis of peripheral blood. The second and the third depletion events were introduced only after > 80% reconstitution was achieved. Gray bars represent the average time for B-cell reconstitution after each depletion, and black bar, the time needed for B-cell reconstitution in young mice. These data summarize the experiments of Keren et al.48
Importantly, the study by Keren et al showed that old mice that have rejuvenated their B lineage on B-cell depletion mount enhanced antibody response to new antigenic challenge.48 As peripheral B cells in aging have intrinsic defects, which limit their immune responsiveness,87 replacing them with new naive B cells confers enhanced immune competence to combat new and evolving pathogens. The ability to rejuvenate the peripheral compartment by depletion of B cells is supported clinically in patients treated with rituximab, which depletes B cells, the reconstituting B cells express a young phenotype88 and a diverse repertoire.89 However, replacing the B lineage only is not sufficient to achieve complete restoration of a “young-like” immune response be-cause age-related defects are also developing in T lineage and innate cells.
Reversing aging in other hematopoietic and nonhematopoietic lineages
Although our studies indicate that the B lineage can be rejuvenated, it is not clear whether a similar approach can be applied clinically for rejuvenation of the T lineage because loss of regulatory T cells induce autoimmune/inflammatory diseases.90 It is also not clear whether the remaining thymic tissue in aging is sufficient to generate many T cells or perhaps can expand to facilitate reactivation of T-cell differentiation. A review article by Lang et al suggests that rejuvenation of T lineage cells can be facilitated using the following strategies: (1) replacement of the old T cells with young T cells by transfusions, (2) reprogramming to extend telomere length and stability, and (3) restoration of thymic microenvironment using growth factors, steroids, and cytokines.76 For example, this may generate in aging a peripheral T-cell compartment with broader repertoire and enhanced cellular immunity. The feasibility to rejuvenate the T lineage is supported clinically in patients with refractory autoimmune diseases that were treated with immunoablation followed by autologous hematopoietic stem cell transplantation.91,92 This treatment induced not only depletion of the autoreactive memory cells but also regenerated a self-tolerant immune system through reprogramming and restoring T lineage regulatory networks.93,94
Finally, the concept of removing old cells to rejuvenate the lineage, which we have initially shown in the B lymphocytes,47,48,95 has recently been validated and observed in nonhematopoietic tissues. The recent study by Baker et al96 has used a biomarker for senescence, p16Ink4a to generate a novel transgenic mouse model that allows inducible elimination of p16Ink4a-positive senescent cells. This transgenic system was bred on a BubR1 hypomorphic (BubR1H/H) genetic background, which has a markedly shortened life span and exhibits a variety of age-related phenotypes.97 In this study, Baker et al looked at adipose tissue, skeletal muscle, and the eye, tissues where p16Ink4a is known to contribute to the acquisition of age-related pathologies.98 When these mice were depleted of p16Ink4a-positive cells (starting at 3 weeks of age), there was a substantial delay in the onset of age-related sarcopenia, cataracts, and loss of adipose tissue. Moreover, removal of p16Ink4a-positive cells, even at a later time when age-related phenotypes are apparent in BubR1H/H mice (eg, at 5 months), resulted in an attenuated progression of most of these pathologies. Hence, this study supports the idea that age-related alterations are mediated by genetic changes in senescent cells, possibly induced through the secretion of a yet unidentified cross-talk mediator. The ability to inhibit or even to reverse these changes, as shown in hematopoietic47,48 and nonhematopoietic lineages,96 indicates that the aging process can be regulated.
Potential impact of reversing age-related deteriorations
With increasing life expectancy, it is estimated that by 2050 almost 40% of the European and United States populations will be > 60 years old.99 The increasing prevalence and severity of infectious diseases30 among the elderly population have a significant negative impact on quality of life and increase dependency on healthcare systems. Attempts to improve vaccination efficacy among elderly populations has had only limited success,100 indicating that new innovative approaches are necessary to enhance immune competence and avoid cellular senescence in aging. A major limitation for these attempts is the composition of the different cellular compartments in aging, which can have poor responsiveness72 and a limited repertoire.67,68 The dogma that these age-related changes are progressive and irreversible must now be changed to take into consideration the recent findings showing reactivation and rejuvenation in hematopoietic and nonhematopoietic tissues obtained by removal of the senescent cells. How signals from senescent cells promote age-related disorders or regulate cellular homeostasis remains unknown. However, recent proof-of-principle experiments suggest a novel therapeutic intervention for treatment or delaying age-related disorders, thus conferring healthy human life in aging. In the immune system, this approach may reduce frequencies and severity of infectious diseases among the elderly population and increase resistance to new or evolving pathogens. It may eventually be translated not only to improving quality of life, but also to reducing Medicare costs. The potential impact of this approach is yet to be evaluated in an appropriate clinical study.
Acknowledgments
The authors thank Patrick Adair for a critical reading of the manuscript.
This work was supported by the Israel Science Foundation (grant 1024/09), the FIRST Program (grant 1362/11), and the Weisz Research Found in Gerontology (all to D.M.). D.W.S. was supported in part by the National Institutes of Health (grants AI035622 and HL061883) and the Uniformed Services University of the Health Sciences.
National Institutes of Health
Authorship
Contribution: D.M. and D.W.S. wrote and edited the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Doron Melamed, Technion, Faculty of Medicine, Department of Immunology, Haifa 31096, Israel; e-mail: melamedd@tx.technion.ac.il.