Abstract
Abstract 841 FN2
FN2
High-intensity therapeutic exposures and prolonged immunosuppression increase the risk of long-term complications after HCT, with an attendant increase in the healthcare needs of these long-term survivors. We have previously demonstrated that morbidity increases with increasing time after HCT (Sun CL, Blood, 2010;116:3129–39). However, the burden of morbidity in patients who survive extended lengths of time after HCT and the consequent healthcare needs of these survivors are unknown.
Utilizing resources offered by the BMTSS, we evaluated the risk of chronic health conditions and psychological health of 366 10+ year HCT survivors and their siblings (n=309). A severity score (grade 1 [mild]; grade 2 [moderate], grade 3[severe], grade 4 [life-threatening], and grade 5 [death due to chronic health condition]) was assigned to each health condition using the CTCAE, v3.0. Cumulative incidence of chronic health conditions was evaluated, using competing risks method. Brief Symptom Inventory (BSI) was used to describe adverse psychological health. Multivariate regression analysis allowed identification of vulnerable subgroups. The current status of healthcare utilization by the HCT survivors was also evaluated.
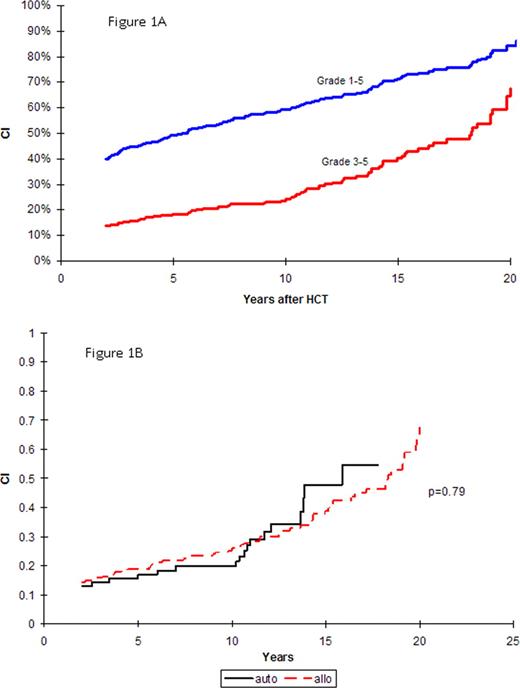
The mean age at HCT was 22 years (range: 0.4–59.8) and at study participation was 37 years (range: 11–72); mean length of follow-up was 15 years (range: 10–28). Primary diagnoses included AML (28%), ALL (17%), CML (17%), NHL (11%), aplastic anemia (11%), HL (7%), and other diagnoses (9%). Stem cell graft was autologous (27%); allogeneic related (65%) and unrelated donor (8%); 72% of the patients received TBI-based conditioning. At least one chronic health condition was reported by 74% of the HCT survivors, compared with 29% of siblings (p<0.001); 25% of the survivors reported severe/life-threatening conditions compared to only 8% of the siblings (p<0.001). Commonly reported severe/life-threatening chronic health conditions included myocardial infarction, stroke, blindness, diabetes, musculoskeletal problems, and subsequent malignancies. As shown in Figure 1A, the 15-year cumulative incidence of any chronic health condition (grades 1–5) was 71% (95% CI, 67–75%), and of severe-life-threatening conditions or death was 40% (95% CI, 33–47%). HCT survivors were 5.6 times as likely to develop a severe/life-threatening condition (95% CI, 3.7–8.6), compared with age- and sex-matched siblings. The cumulative incidence of severe/life-threatening conditions did not differ by type of HCT (p=0.79, Figure 1B). Using BSI, we evaluated somatic distress, anxiety, and depression among HCT survivors and their siblings. While the prevalence of anxiety and depression were comparable between survivors and siblings, HCT survivors were 2.7 times more likely to report somatic distress (p<0.001). Among survivors, female gender (OR=3.6, 95% CI, 1.4–9.0), low household income (<$20,000 OR=4.4, 95% CI, 1.1–17.2), and poor self-rated health status (OR=10.6, 95% CI, 4.0–27.9) were associated with increased risk for somatic distress. Fortunately, 90% of HCT survivors carried health insurance coverage, because a high proportion needed ongoing specialized medical care; 69% of the HCT survivors reported cancer/HCT-related visits at an average of 15 years after HCT.
The burden of long-term physical and emotional morbidity borne by 10+ year HCT survivors is substantial, resulting in a high utilization of specialized healthcare. Patients, families and healthcare providers need to be made aware of the high burden, such that they can plan for post-HCT care, even many years after HCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal