Abstract
Abstract 666
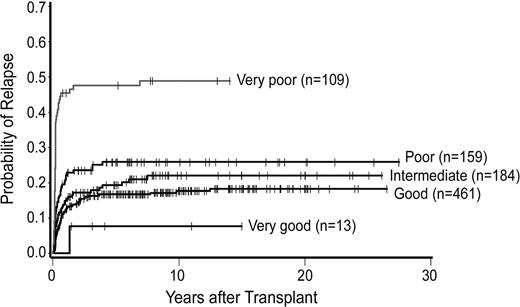
The success of HCT for myelodysplastic syndrome (MDS) is hampered by regimen-related toxicity and relapse. Relapse is dependent primarily upon the patient's clonal karyotype, generally classified by IPSS into 3 groups: good, intermediate, and poor. Schanz et al. proposed a new classification that distinguishes 5 cytogenetic risk groups, very good, good, intermediate, poor and very poor, with median survivals in non-transplanted patients ranging from 61 to 6 months. Here, we determined the impact of these novel risk categories on post-HCT outcome.
We analyzed results in 1042 patients with MDS (including progression to acute myeloid leukemia [tAML]) transplanted at the FHCRC; 89% of HCT were carried out since 1990. Patients were 1–75 (median 45) years old and were prepared for HCT with various high-dose or reduced/low-intensity conditioning regimens. Donors were related (54%) or unrelated (46%); the source of stem cells was marrow (52%) or G-CSF mobilized peripheral blood progenitor cells (PBPC; 48%). The association of the 5-group cytogenetic classification with HCT outcome was examined in univariate and multivariate analyses.
The 3-year probabilities of relapse with very good/good/intermediate/poor/very poor cytogenetics were 8%, 17%, 19%, 26% and 48%, and overall survivals were 46%, 46%, 41%, 37% and 8%, respectively. Hazard ratios (HR) from univariate analysis are shown in the table.
| Variable . | Category . | Hazard Ratio (HR)/CI . | P= . |
|---|---|---|---|
| Mortality | |||
| Very good | 1.06/0.50–2.24 | 0.89 | |
| Good | 1 | – | |
| Intermediate | 1.22/0.97–1.52 | 0.08 | |
| Poor | 1.35/1.07–1.69 | 0.01 | |
| Very poor | 3.13/2.47–3.96 | <0.0001 | |
| Relapse | |||
| Very good | 0.49/0.07–3.56 | 0.48 | |
| Good | 1 | – | |
| Intermediate | 1.38/0.94–2.05 | 0.10 | |
| Poor | 1.83/1.25–2.68 | 0.002 | |
| Very poor | 7.46/5.20–10.69 | <0.0001 |
| Variable . | Category . | Hazard Ratio (HR)/CI . | P= . |
|---|---|---|---|
| Mortality | |||
| Very good | 1.06/0.50–2.24 | 0.89 | |
| Good | 1 | – | |
| Intermediate | 1.22/0.97–1.52 | 0.08 | |
| Poor | 1.35/1.07–1.69 | 0.01 | |
| Very poor | 3.13/2.47–3.96 | <0.0001 | |
| Relapse | |||
| Very good | 0.49/0.07–3.56 | 0.48 | |
| Good | 1 | – | |
| Intermediate | 1.38/0.94–2.05 | 0.10 | |
| Poor | 1.83/1.25–2.68 | 0.002 | |
| Very poor | 7.46/5.20–10.69 | <0.0001 |
While the impact of the 5-group cytogenetic risks “good” and “intermediate” coincided almost entirely with the IPSS cytogenetic risk groups “good” (98%) and “intermediate” (83%) respectively, the third IPSS group, “poor”, was split into the categories “intermediate” (13%), “poor” (50%) and “very poor” (36%) in the novel 5-group classification. Among patients in IPSS cytogenetic risk group “poor”, the 5-group category “very poor” had significantly worse outcome (HR=2.82 [1.78-4.46, p<.0001] for mortality; HR=3.57 [1.85-6.88, p=.0002] for relapse); outcome for the “poor” group was similar to the “intermediate” risk category in the 5-group classification (HR=1.17 [0.74-1.85, p=.49) for mortality; HR=0.99 [0.50-1.92, p=.96] for relapse). The group “very good” showed a HR of 0.494 for relapse, but with only 13 patients the difference to the “good” group was not statistically significant. Consistent with the IPSS, increasing blasts were associated with an increased risk of mortality (p=.007) and relapse (p<.0001) after adjusting for cytogenetic risk by the new 5-group classification. In addition, increasing platelet counts were associated with lower mortality (p=.0006) but not relapse (p=.85). After adjusting for cytogenetic risk and the factors listed above, increasing age was associated with a higher rate of mortality (p<.0001) but not relapse (p=.87). The risk of mortality was decreased in more recent years of HCT (p<.0001). Patients with unrelated donors had a higher rate of mortality compared to those with HLA matched-sibling donors (HR=1.34, p=.005), but also tended to have a lower relapse risk (HR=0.74, p=.08). The associations of the new 5-group karyotype categories with outcome were similar to those listed above when these other factors were not adjusted for.
The present data confirm the profound impact of cytogenetic risk on post-HCT relapse and mortality in patients with MDS and indicate that the newly proposed classification distinguishes different risk cohorts even more clearly than the original IPSS classification. In fact, for both overall mortality and relapse the 5-group model significantly improves the previous model of only three cytogenetic risk groups (p<0.0001 for both endpoints). The data indicate, furthermore, that patient age, platelet counts, and donor type significantly impact transplant outcome. Finally, results show that outcomes with HCT in patients with MDS have improved over the years. Future trials must focus on conditioning regimens that allow to reduce non-relapse mortality in patients with low risk cytogenetics and reduce relapse incidence in patients with high-risk karyotypes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal