Abstract
Abstract 503
Extranodal NK/T-cell lymphoma, nasal type (ENKL) is a rare subtype of lymphoma and its standard therapy is not established. The response to conventional chemotherapy is not good, resulting in generally poor prognosis. Hematopoietic stem cell transplantation (HSCT) is a promising strategy, but no large-series studies were presented.
The Lymphoma Working Group of JSHCT surveyed the database in Japan and retrospectively analyzed. Of 11,267 transplants for all types of lymphoproliferative disorders, a total of 134 HSCT were conducted for 120 ENKL patients with sufficient data for analysis. The study was performed in accordance with the Declaration of Helsinki and was approved by the JSHCT Ethical Committee and the Institutional Review Boards of Nagoya University.
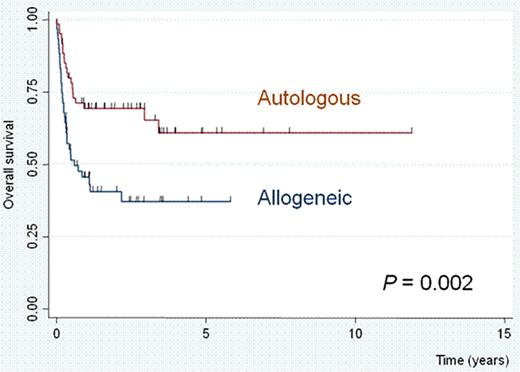
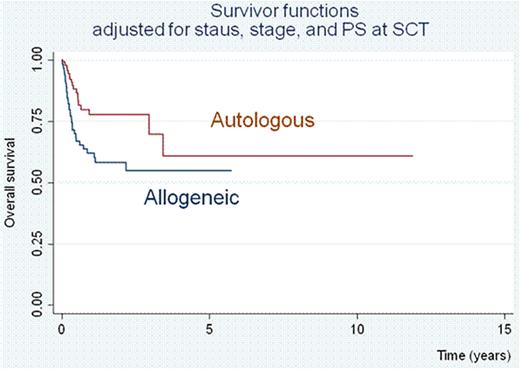
There were 75 male and 45 female with a median age of 47 years (range: 18–70). The median follow-up of survivor was 27 months. In total, 74 patients received allogeneic hematopoietic stem cell transplantation (60 with 1st transplant and 14 with 2nd transplant) and 60 received autologous peripheral blood stem cell transplantation (PBSCT). The donor of allogeneic 1st transplant was relatives in 28, unrelated bone marrow (UR-BM) in 9, and cord blood (CB) in 23. For 1st transplant, 63 patients were in complete response (CR) (41 autologous, 10 relative, 5 UR-BM, and 7 CB), 12 were in partial response (PR) (5 autologous, 4 relative, 1 UR-BM, and 2 CB), and 45 were on disease (14 autologous, 13 relative, 4 UR-BM, and 14 CB). For patients who received allogeneic transplant, 38 (64%) were in stage IV at initial presentation, while only 20 (33%) were in stage IV for patients who received auto-transplant. The proportion of low international prognostic index was also different between allo-transplant (34%) and auto-transplant (62%) groups. The 2-year overall survival (OS) was significantly better for those received auto-transplant than allo-transplant (69% vs. 41%, Figure 1). The OS of patients who received 2nd transplant was 27% at a median follow-up of 18 months. Multivariate analysis showed that three factors (initial stage IV, non-CR status and performance status at transplant) were significant factors associated with poor prognosis, but the type of transplant (autologous or allogeneic) was not. By adjusting above three factors, the difference between autologous and allogeneic transplant was minimized (Figure 2).
Prognosis of ENKL patients who received autologous transplant was better than that of allogeneic transplant, partly due to the selection that patients in good condition tended to receive auto-transplant. In another words, for patients with good condition, autologous HSCT is a good treatment choice. Any type of HSCT is a potential option for ENKL patients in non-CR. The 2nd SCT is beneficial for a part of patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal