Abstract
Abstract 4480
Adult T-cell leukemia (ATL) endemic in southwestern Japan is an HTLV-I-induced mature T-cell neoplasm. It has a dismal prognosis when treated with conventional chemotherapy, mainly because ATL cells overexpress multidrug-resistance genes. Allogeneic hematopoietic stem cell transplantation (allo-SCT) has been reported to improve the prognosis. However, it is also known that allo-SCT shows high treatment-related mortality (TRM) because of disease characteristics of severely deteriorated cellular immunity. Therefore, we evaluated the outcome of reduced-intensity stem cell transplantation (RIST), compared to conventional stem cell transplantation (CST) for ATL patients (pts).
We retrospectively analyzed consecutive 20 pts with aggressive ATL (acute type, 16; lymphoma type, 4) who underwent allo-SCT between 2000 and 2010 in our institute. The age of pts who received RIST was significantly older than that of CST (P = <.001). The other parameters were balanced between the two groups (Table 1).
All pts received induction chemotherapy with Japan Clinical Oncology Group (VCAP-AMP-VECP) regimen or biweekly CHOP prior to SCT. Nine pts received a conventional myeloablative conditioning with CY/TBI-based (n=8) or BU/CY-based (n=1) regimens and 11 pts received a reduced-intensity regimen with fludarabine(Flu)/melphalan(Mel)±TBI (Flu 25 mg/m2 on days -6 to -2 + Mel 40 mg/m2 on days -4 and -3 ± TBI 4 Gy on day -1). Graft-versus-host-disease (GVHD) prophylaxis consisted of cyclosporine plus short-term methotrexate (sMTX) for HLA-matched sibling donor recipients and tacrolimus plus sMTX for the others. Cyclosporine or tacrolimus was promptly tapered when complete chimerism was achieved.
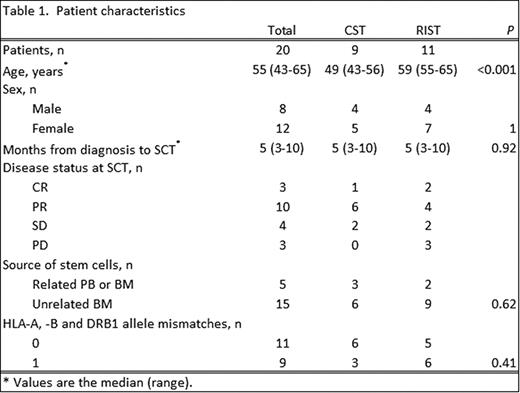
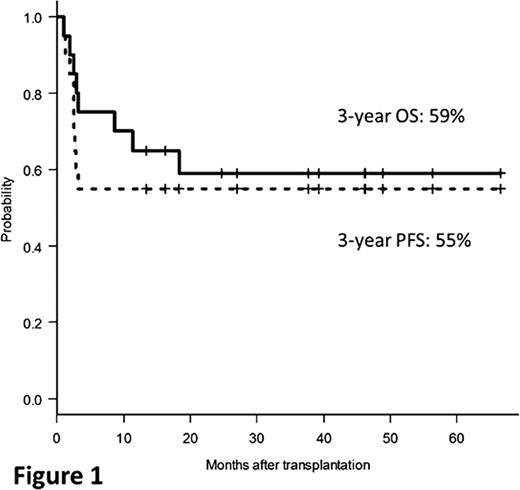
The estimated 3-year overall survival (OS) and 3-year progression-free survival (PFS) rates for all pts were 59% and 55%, respectively (Fig. 1). At the median follow-up duration of 25 months (1–67), 12 pts were alive and 8 pts dead. Causes of death were disease progression (n=4) and treatment-related complications including acute GVHD and infection (n=4). The cumulative incidences of disease-associated mortality and TRM at 3 years were 21% and 20%, respectively. Importantly, after 1 year post-transplantation, the curve of PFS reached plateau phase. Therefore, allo-SCT could be a curable therapeutic option for aggressive ATL.
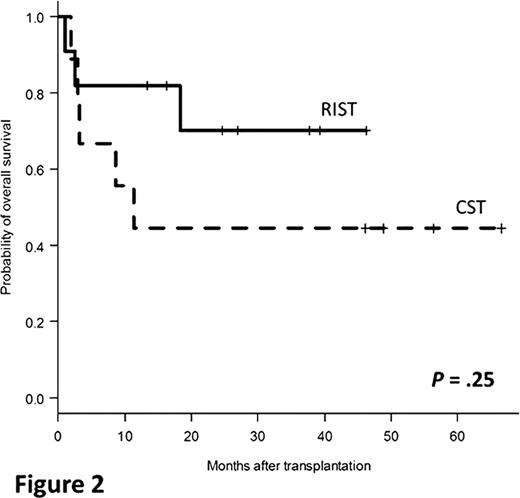
It is notable that RIST showed excellent 3-year OS. Although not significant, 3-year OS for RIST and CST were 70% and 44% (P =.25), respectively (Fig. 2). TRM of RIST trended to be low compared with that of CST (18% vs 22%, P =.87). In addition, chronic GVHD was observed in 91% of the evaluable 11 pts (limited type, 6; extensive type, 5). It is suggested that both improvement of TRM and the induction of graft-versus-leukemia effects may contribute to the favorable outcome in RIST for ATL. Furthermore, it should be stressed that older pts who preferentially received RIST rather than CST achieved favorable survival comparable to younger pts (≥ 50 years: 58% vs < 50 years: 60%, P =.94). We would suggest that RIST should be applied to all ATL pts eligible for allo-SCT, regardless of the age.
Univariate analysis for all pts revealed that only male sexuality was a significant poor prognostic factor for OS (male: 25% vs female: 82%, P =.006). Regarding disease status at SCT, CR or non-CR did not significantly affect OS (CR: 67% vs non-CR: 58%, P =.98). However, PD was an adverse impact on 3-year OS (PD: 33% vs non-PD: 64%, P =.11). It is recommended that ATL pts receive allo-SCT in early phase before the disease becomes chemo-resistant, even if they do not achieve CR.
Allo-SCT for ATL remarkably improved the poor prognosis. Especially, RIST is a promising procedure for excellent outcome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal