Abstract
Abstract 4481
HLA matching has been demonstrated to play a major role in the different outcomes of allogeneic hematopoietic transplantation (allo-HSCT) in patients with hematological malignancies. When searching for an unrelated donor the commonly evaluated HLA loci are -A, -B, ± -C, -DRB1 and DQB1. The 2 loci DRB3 and DRB4 have never been taken into account and never been evaluated.
To evaluate the impact of HLA-DRB3 and -DRB4 on the different unrelated allo-HSCT outcomes especially in case of mismatch presence on these loci.
We have of 30 patients (study group) who received unrelated allo-HSCT with a HLA-DRB3 or HLA-DRB4 mismatched donor and we compared their outcomes to outcomes of a matched control group of 30 patients with the same characteristics except for the DRB3 or DRB4 donor mismatching. In the study group, there were 16 males and 14 females with a median age of 45 years (25–62), 18 patients had AML, 6 ALL, 2 MDS, 2 multiple myeloma (MM), 1 CML and 1 NHL. Fifteen patients received a myeloablative conditioning and 15 received a reduced intensity one (RIC). At transplantation, 16 patients were in CR, 4 in PR and 10 in relapse; 15 patients received PBSC and 15 BM. There were 16 patients with 10/10 HLA identical donor among them 11 had a DRB3 mismatch and 5 had a DRB4 mismatch. There were 14 patients with 9/10 HLA identical donor among them 9 had a DRB3 mismatch (mismatched: 3 on HLA-A, 1HLA-B, 4 HLA-C and 1 on HLA-DQB1) and 5 had a DRB4 mismatch (mismatched: 1 on HLA-A, 1HLA-B, 1 HLA-C and 2 on HLA-DQB1). In the control group, there were 16 males and 14 females with a median age of 46 years (25–64), 18 patients had AML, 6 ALL, 3 MM, 1 CML and 2 NHL. Fifteen patients received a myeloablative conditioning and 15 received a RIC. At transplantation, 22 patients were in CR, 1 in PR and 7 in relapse; 15 patients received PBSC and 15 received BM. There were 16 patients with 10/10 HLA identical donor and 14 patients with 9/10 HLA identical donor (mismatched: 6 on HLA-A, 3 HLA-B, 4 HLA-C and 1 on HLA-DQB1) all patients in the control group were matched for HLA-DRB3 and –DRB4.
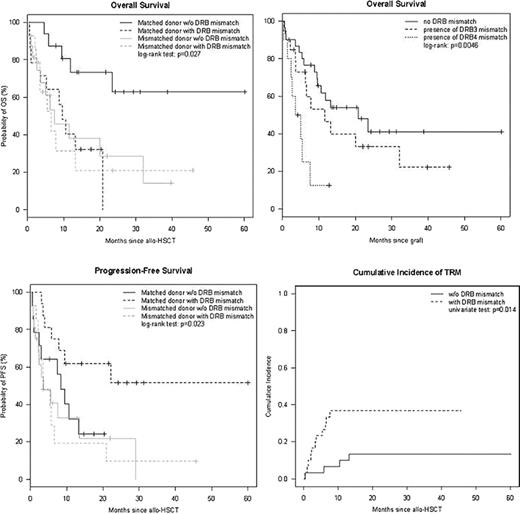
After HSCT, 27 (90%) patients in the study group engrafted while 29 (96%) engrafted in the control group. The cumulative incidence of acute GVHD≥2 at 3 months was 37% (28–46) and 30% (22–39) for the study and control groups respectively, with a same cumulative incidence of chronic GVHD at one year of 20% (12–28). At day 90 post HSCT, 17 (63%) patients in the study group were in CR and 25 (86%) in CR in the control group. After a median follow-up of 5 months (0.2–46) and 13 months (0.5–60) for study and control groups respectively, the median overall survival (OS) was 7 months (3–32) and 21 months (11-NR) with a 2-years probability of 25% (12–51) and 41% (25–69) respectively; the median time of progression-free survival (PFS) was 3 months (0.2–46) and 10 months (1–60) with a 2-years probability of 16% (6–42) and 37% (21–63) respectively. The cumulative incidence of relapse at 1 year was the same for the two groups with 30% (22–39); the cumulative incidence of transplant related mortality (TRM) at 3 months and 1 year were 17% (10–24) vs. 3% (0–7) and 37% (28–46) vs. 10% (5–16) for study and control groups respectively. The multivariate analysis that studied age, type of disease, matched or mismatched HLA, with or without DRB3 or DRB4 mismatch, disease status at transplantation and type of conditioning showed a significant worse OS in 9/10 mismatched patients with or without a DRB3 or DRB4 mismatch (HR=5.3; [1.6–18] p=0.006); 10/10 matched patients with a DRB3 or DRB4 mismatch (HR=3.9; [1.2–12] p=0.02) and patients not in CR at transplantation (HR= 4.4; [1.6–12] p=0.004); similarly, the same groups had a worse PFS while patients not in CR or with a DRB3 or DRB4 mismatch showed a worse TRM in multivariate analysis, (HR=6; [1.5–24] p= 0.02) and (HR=3.5; [1.02–12] p=0.04) respectively.
We demonstrated that the HLA-DRB3 or DRB4 matching donor is relevant for OS and TRM of patients who undergo allo-HSCT from unrelated donor either in the 10/10 or 9/10 HLA matching settings. Moreover, in view of the important impact of these loci mismatches, we recommend its consideration in the unrelated donor selection setting particularly in the 10/10 HLA unrelated donors. Since the evaluation of these loci is not widely done within HLA laboratories, we suggest conducting a large prospective study in order to validate its impact on unrelated allo-HSCT outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal