Abstract
Abstract 4119
The outcome of multiple myeloma (MM) has improved significantly over the last 2 decades due to the availability of several novel agents and an increasing use of high-dose chemotherapy and autologous hematopoietic stem cell transplant (auto-HCT). There is considerable evidence that the response to induction therapy predicts a favorable outcome after high-dose chemotherapy and auto-HCT. In this report, we evaluated the impact of pre-transplant response to conventional agents on post auto-HCT outcomes including time to progression (TTP), progression free survival (PFS) and overall survival (OS).
1567 patients received auto-HCT at UT-MD Anderson Cancer Center between 1988 and December 2010. Pre auto-HCT disease status was divided into the following prior auto-HCT response groups: complete response (CR), very good partial response (VGPR), partial response (PR), minor response (MR), stable disease (SD) and progressive Disease (PD). The primary objective was to study the impact of prior response on the outcome. Demographics, disease-related and transplant-related variables were collected. The distributions of TTP, PFS and OS were estimated by the Kaplan-Meier method. Log-rank test was performed to test the difference in survival between groups. Regression analyses of survival data was based on the univariate and multivariate Cox proportional hazards model.
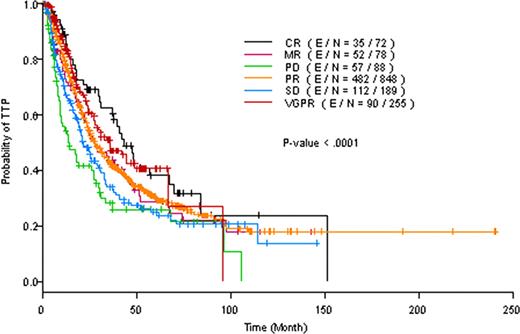
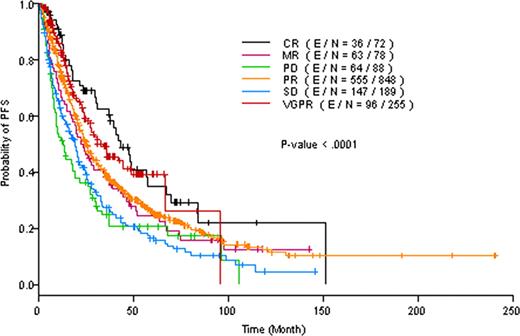
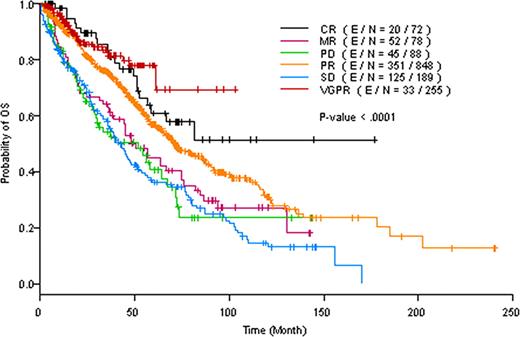
Median age at auto-HCT was 56.8 years. Median time from diagnosis to auto-HCT was 7.9 months. Of the 1567 patients, 72 (4.6%) achieved CR before auto-HCT, 255 (16%) had VGPR, 848 (54%) had PR, 78 (5%) had MR, 189 (12%) had SD, 88 (5.6%) had PD, while the response was unknown in 37 (2%) patients. Almost 17% patients were 65 years or older at auto-HCT and approximately 7% had high-risk cytogenetic abnormalities. On univariate analysis, the response prior to auto-HCT had significant impact on TTP (p=<0.0001), PFS (p=<0.0001), and OS (p=<0.0001), In multivariate models, the response prior to auto-HCT still emerged as a significant predictor of TTP, PFS and OS (p =0.0055, p=0.0004 and p<0.0001, respectively) after adjusting for percent of plasma cells, time interval from diagnosis to transplantation and/ or creatinine level. In particular, patients who achieved CR prior to auto-HCT had significantly longer TTP, PFS and OS when compared to patients who had PR, MR, SD or PD (Figures 1–Fig 3). In contrast, TTP, PFS and OS were not significantly different between patients who achieved a CR or VGPR prior to auto-HCT.
Patient who achieved CR or VGPR before undergoing an auto-HCT had significantly longer TTP, PFS and OS after the transplant. These results highlight the importance of effective anti-myeloma therapy to maximize the response before proceeding to auto-HCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal