Abstract
Survival in primary myelofibrosis (PMF) is assessed by the Dynamic International Prognostic Scoring System (DIPSS) (Blood 2010;115:1703) and DIPSS-plus (JCO 2011;29:392). The latter is based on eight risk factors including age>65 years, constitutional symptoms, hemoglobin <10 g/dL, red blood cell transfusion need, leukocyte count >25 × 109/L, platelet count <100 × 109/L, peripheral blood (PB) blasts ≥1% and unfavorable karyotype. Recent studies have highlighted the prognostic significance of monosomal karyotype (MK) (Blood 2011;117:5612), unfavorable karyotype (Leukemia 2011;25:82) and platelet count <100 × 109/L ((JCO 2011;29:392), for leukemic transformation (LT) in PMF.
A combination of multivariable and receiver operating characteristic (ROC) analyses were applied to a Mayo Clinic database of 884 karyotypically-annotated patients with PMF, in order to define karyotype-dependent and karyotype-independent risk models for LT. The karyotype-independent model was further validated in a separate cohort of 525 PMF patients from an international database (Blood 2010;115:1703). Patients in the Mayo cohort were evaluated at time of referral and those of the international database at time of initial diagnosis.
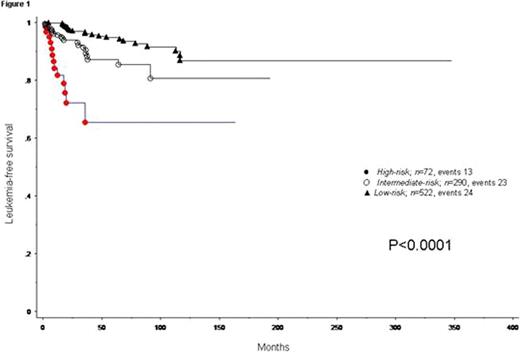
Sixty cases of LT were documented. Karyotype (categorized into MK, inv(3)/i(17q) abnormalities, other unfavorable, and favorable), PB blast percentage (as a continuous variable), and platelet count (as a continuous variable) were the most reliable (p<0.01) in predicting leukemia-free survival (LFS). The best discriminant levels for inferior LFS were MK (HR 6.2, 95% CI 2.2–17.1), inv(3)/i(17q) abnormalities (HR 7.6, 95% CI 1.8–33.3), PB blast ≥2% (HR 2.4, 95% CI 1.4–4.2) and platelet count ≤41 × 109/L (HR 2.6, 95% CI 1.3–5.1). MK and inv(3)/i(17q) abnormalities were subsequently consolidated into one “very high risk” cytogenetic category (n =27), with a corresponding HR of 6.6 (95% CI 2.7–16.0). HR-based risk scores were assigned to “very high risk” karyotype (2 points), PB blast ≥2% (one point) and platelet count ≤50 × 109/L (one point) to classify patients into low (no adverse points; n =522), intermediate (one adverse point; n =290) and high risk (two or more adverse points; n =72) groups; the corresponding 3-year LT rates were 3%, 10% (HR 2.6; 95% CI 1.4–4.6) and 35% (HR 9.4, 95% CI 4.7–18.7) (Figure 1).
The karyotype-independent model was based on PB blast percentage and platelet count only; low-risk (no adverse points; n =525), intermediate-risk (one adverse point; n =311) and high-risk (two adverse points; n =48); the corresponding 3-year LT rates were 3%, 12% (HR 3.1, 95% CI 1.8–5.4; p<0.0001) and 25% (HR 6.0, 95% CI 2.6–14.1). The karyotype-independent model was validated in a separate cohort of 525 PMF patients with 70 documented cases of LT, from an international database (Blood 2010;115:1703).
The current leukemia risk models are applicable at diagnosis or during follow-up, in the presence or absence of cytogenetic information, and complement DIPSS-plus in the comprehensive prognostication of patients with PMF.
Vannucchi:Novartis: Honoraria.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal