Abstract
Abstract 360
Preemptive treatments employing antiviral drugs have decreased in cytomegalovirus (CMV) infection. However, CMV has remained one of the most common pathogens causing morbidity and mortality after allogeneic hematopoietic stem cell transplantation (HSCT). Chronic viral infections with several human viruses were shown to be associated with exhausted T cells with high expression of the inhibitory molecule programmed death 1 (PD-1). PD-1 expression on CMV-specific T cells after HSCT has not been well examined. We evaluated the involvement of exhausted CMV-specific T cells characterized by high PD-1 expression in persistent CMV infection after allogeneic HSCT. Although some cytokines, such as IL-10, reportedly upregulate PD-1 expression, what increases PD-1 expression has not been well known. We also aimed to identify soluble factors regulating PD-1 expression on exhausted T cells.
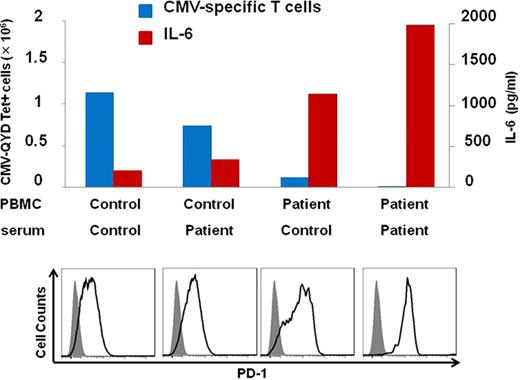
Peripheral blood mononuclear cells (PBMC) and serum were obtained from an HLA-A*2402-positive patient who had received bone marrow transplantation from an HLA-A, B, C and DR matched unrelated donor. This patient failed to eliminate CMV for more than one year after transplantation despite intermittent administration of antiviral drugs. Control PBMC and serum were obtained from an HLA-A*2402-positive healthy volunteer. All blood was collected with written informed consent. We at first analyzed frequencies of CMV-specific CD8+ T cells in patient and control PBMC by flow cytometer using QYDPVAALF/A*2402-specific tetramer and CD8 antibodies. QYDPVAALF is derived from CMV pp65 protein and presented by the HLA-A*2402 molecule. Tetramer-stained cells were detected in patient PBMC but not control PBMC (0.11% versus undetectable). Patient and control PBMC were stimulated by a synthetic peptide QYDPVAALF in culture media containing IL-2 for 14 days, and stained with QYD/A*2402-specific tetramer. Remarkably, post-stimulated patient PBMC contained only 0.54% of tetramer-stained CD8+ T cells, whereas a more dramatic increase (14.1%) was found in control PBMC. We analyzed frequencies of IFN-g secreting CD8+ T cells in PBMC after 4-hour stimulation with a peptide pool covering the whole CMV pp65 protein. Less patient CD8+ T cells produced IFN-g, compared with the control CD8+ T cells (0.1% versus 0.5%). These data demonstrate dysfunction of CMV-specific CD8+ T cells in the patient with persistent CMV infection. To examine the involvement of PD-1 in dysfunction of CMV-specific CD8+ T cells, we analyzed the expression of PD-1 on CMV-specific CD8+ T cells 14 days after stimulation with QYDPVAALF peptide. CMV-specific CD8+ T cells generated from patient PBMC exhibited higher PD-1 expression, compared with CMV-specific CD8+T cells generated from control PBMC. Next, we stimulated patient PBMC with QYDPVAALF peptide for 14 days in the presence or absence of anti-PD-L1 antibody, which blocks PD-1/PD-L1 inhibitory pathway. Blockade of the PD-1/PD-L1 pathway resulted in a 3.9-fold increase in patient CMV-specific T cells. These findings demonstrate that PD-1 is associated with the exhaustion of CMV-specific CD8+ T cells during persistent CMV infection in this patient. Next, to examine the effect of soluble factors on CMV-specific CD8+ T cells, we analyzed the levels of cytokines in patient and control sera by multiplex bead assay. Patient serum exhibited a higher IL-6 level compared with control serum. We stimulated patient and control PBMC with QYDPVAALF peptide for 14 days in culture media with patient or control serum. Patient serum led to poorer growth and higher PD-1 expression of CMV-specific CD8+ T cells. In addition, as the growth of CMV-specific CD8+ T cells was worse, the IL-6 level in the supernatant was higher (Fig). Blockade of IL-6/IL-6 receptor interaction using anti-IL-6 receptor antibody resulted in a 5-fold increase in patient CMV-specific T cells. We analyzed the IL-6 concentration in sera from healthy donors (n=5) and patients with temporary (n=4) and persistent (n=3) CMV infection after allogeneic HSCT. Serum from patients with persistent CMV infection showed a significantly higher IL-6 level. These findings suggest that IL-6 was associated with exhaustion of CMV- specific T cells.
Naoe:Dainipponn-Sumitomo Pharma.: Research Funding; Chugai Pharma.: Research Funding; Novartis Pharma.: Honoraria, Speakers Bureau; Zenyaku-Kogyo: Research Funding; Otsuka Pharma.: Research Funding; Kyowa-Hakko Kirin.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal