Abstract
Iron overload is frequent in patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT) due to multiple red blood cell transfusions in the pre- and post-transplant period. Serum ferritin is a routine marker for iron overload. Along with transferrin saturation and soluble transferrin receptor, it was recently shown to strongly impact on survival after HSCT. Reduction of iron overload – e.g. by chelation - might improve the outcome after allogeneic transplantation. To analyze whether patients might benefit from post-transplant interventions aimed at reducing iron overload, we evaluated the impact of iron parameters on survival in a cohort of patients in which complete iron parameters were assessed before and at multiple time-points after transplantation.
We studied 153 consecutive patients undergoing unmanipulated T-cell replete allogeneic transplantation at our center between 2005 and 2009. Among 90 males and 63 females with a median age of 46.5 years (range 18 – 70 years), underlying diseases were AML/MDS (n=87), ALL (n=25), lymphoma/myeloma (n=25), CML/MPN (n=12) and non-malignant (n=4). Donors were HLA-identical (n=78) or one-antigen mismatched (n=2) siblings, or unrelated volunteer donors (n=73). Patients with lymphoma received conditioning with BEAM, fludarabine and single dose total body irradiation (TBI). All other patients were treated with cyclophosphamide and busulfan, or cyclophosphamide and TBI +/− etoposide. Graft-vs-host disease prophylaxis was with Cylosporin A plus either methotrexate or mycophenolate. Serum iron parameters including ferritin, transferrin saturation, transferrin, iron and soluble transferrin receptor (sTfR) were determined before HSCT as well as 3, 6, 12, 24, 36 and 60 months post-transplant. Patients were categorized into groups with high or low iron parameters according to values above or below median at each time-point. Predictors of transplant outcome were further evaluated in multivariable Cox models using disease and stage as covariates.
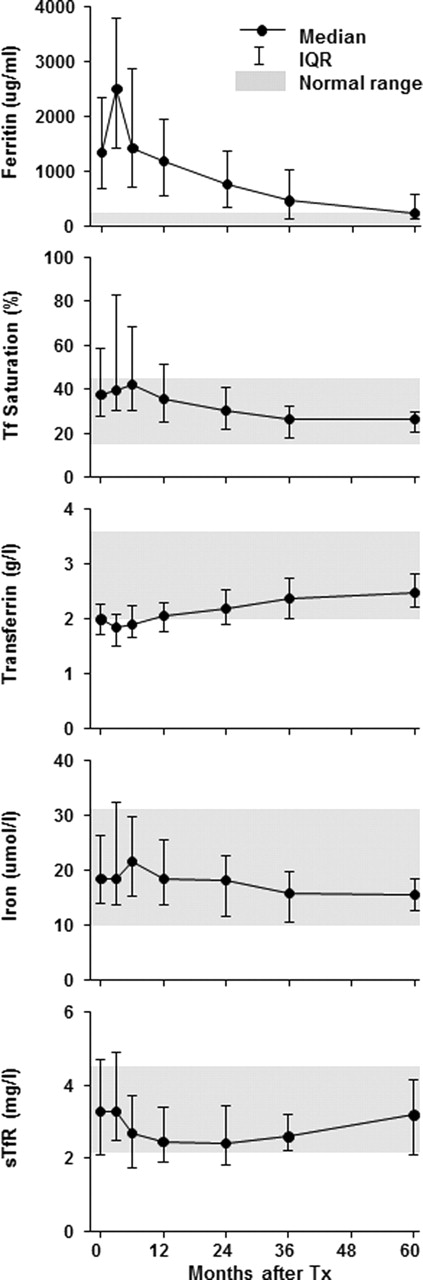
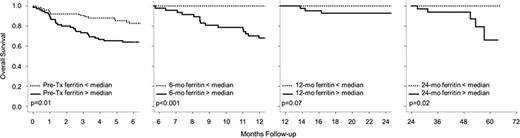
Of the 153 patients, 83 were alive at last contact with a median follow-up of 3.4 years. Ferritin was strongly elevated before HSCT (median 1344 ng/ml, range 16–6507 ng/ml), peaked 3 months post-transplant (median 2508 ng/ml, range 71–9756 ng/ml) and continuously decreased to reach values within the normal range at 5 years (median 242.5 ng/ml, range 28–984ng/ml). Transferrin saturation and iron analogously peaked in the early post-transplant period and subsequently lowered, while transferrin and sTfR increased after an early post-transplant nadir up to 5 years. The post-transplant course of all iron parameters is shown in Fig 1. As demonstrated previously, survival analysis showed a poor survival of patients with a pre-transplant ferritin value above the median (hazard ratio 2.4, p=0.001). Time-stratified landmark survival analysis showed that iron overload (as assessed by ferritin levels above the median at the respective time-point) had a detrimental effect on survival in all periods analyzed (0–6 months p=0.01; 6–12 months p<0.001; 1–2 years p=0.07; and 2–5 years p=0.02. Figure 2). Interestingly, no patient with a ferritin level below the median died more than six months post-transplant. Excess mortality in patients with high ferritin was due to increased transplant related mortality. After adjustment for disease and stage, elevated ferritin values retained their prognostic significance. Analysis of the other iron parameters showed similar trends, but their prognostic value was lower than that of ferritin.
Iron overload before HSCT as well as during the post-transplant follow-up confers an increased risk of death. Iron parameters significantly impact on survival during all post-transplant intervals analyzed. Thus, our data suggest that patients may benefit from interventions to reduce iron overload after HSCT.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal