Abstract
Patients with refractory immune thrombocytopenia (ITP) have limited therapeutic options, with morbidity and mortality as often from infection as from bleeding. Thrombopoietin (TPO) mimetics allow an increase in the platelet count without causing immunosuppression. These agents may be especially useful in patients with secondary forms of ITP. We report three patients treated with TPO agonists for ITP post Allogeneic Stem Cell Transplants (SCT).
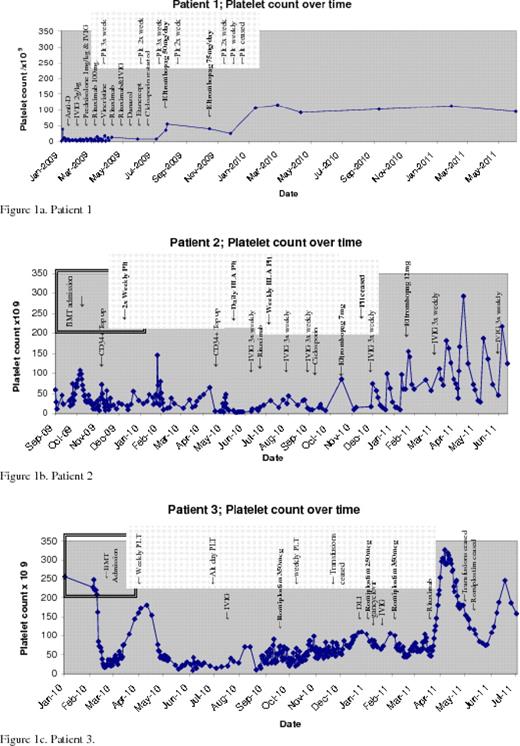
Patient 2: BT, 4yrs(12kg), underwent a myeloablative allogeneic PBSCT in September 2009 for JIA/HLH. She became thrombocytopenic in June 2010, presumed to be ITP. She had no response to prednisolone or rituximab and a only a minimal response to IVIG; requiring platelets 1x weekly. She started Eltrombopag 7mg OD in November 2010, escalated to 12mg by February 2011. This had a synergistic effect with IVIG and she became platelet independent after one month of Eltrombopag and IVIG, maintaining platelet counts 50–200 (figure1b).
Patient 3: MG, 62yrs, underwent a reduced intensity allogeneic SCT in March 2010 for stage 3 Sezary syndrome. Post SCT he developed pancytopenia associated with EBV reactivation. He received daily GCSF, regular blood and weekly platelet transfusions. In July he developed GI bleeding from HSV colitis and his platelet transfusion requirements increased to alternate days. In October 2010 he was started on Romiplostim 250mcg, increased to 350mcg weekly, erythropoetin and GCSF. He had a clinically significant rise in his platelet counts and a reduction in his platelet requirements to 1x weekly within weeks of starting romiplostim. By December he was platelet independent, with counts persistently over 50, and romiplostim was stopped (figure1c).
All three patients remain in remission at the time of submission of the abstract.
Immune cytopenias are well-recognised post myeloablative allografts occurring in 5–37% of SCT recipients. The occurrence of ITP in SCT recipients has been reported, in which GVHD or the production of anti-platelet alloantibodies of recipient origin was considered to play major roles. Although small numbers, these case studies show efficacy of thrombopoietic agents (recently licensed for use in chronic ITP) in patients with thrombocytopenia post SCT refractory to standard therapies, with an early reduction and subsequent cessation in platelet transfusion requirements in all three patients. The lack of immune suppression with these agents may be particularly relevant in patients post SCT, in whom immune reconstitution is vital not only in preventing infections, but also in preventing rejection of the graft and in establishing a graft versus leukaemia effect. Given that TPO receptors are present on haematopoietic stem cells at all stages of development and that TPO provides a growth factor for stem cells, the use of these agents in patients treated for leukaemia requires caution. There was no evidence of progression of disease in these patients and TPO agents were only required for a period of time (patient 3 is off therapy and the others only receive minimal doses). Formal evaluation of these agents in allogeneic SCT is warranted.
Cooper:GSK: Honoraria; Amgen: Honoraria.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal