Abstract
Abstract 309
Despite decades of intensive research, graft vs. host disease (GVHD) remains a major complication of allogeneic transplantation. Much progress has been made toward understanding GVHD pathophysiology and the mechanisms regulating the donor immune response, however no factors have been identified to regulate the response of transplant recipients to GVHD and its concomitant damage. Furthermore, virtually all strategies available to reduce clinical GVHD do so by limiting the donor immune system at the expense of therapeutic graft vs. leukemia/lymphoma (GVL) responses. IL-22 is a recently characterized cytokine that is produced by both helper T cells and innate lymphoid cells (ILC). Expression of its receptor (IL-22R) is generally limited to epithelial and other non-hematopoietic cells, and it has demonstrated a protective role for intestinal epithelium during experimental colitis, providing a signal for intestinal epithelial cell survival, proliferation, and wound healing.
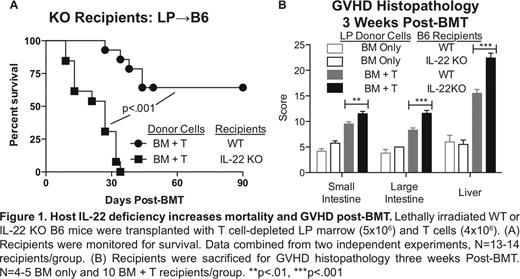
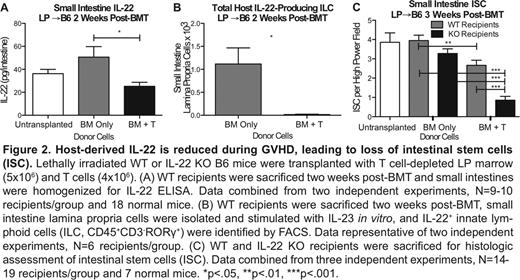
We investigated the role of IL-22 in GVHD during MHC-mismatched C57BL/6 (B6) into BALB/c murine bone marrow transplantation (BMT). Elimination of IL-22 with anti-IL-22 neutralizing antibody lead to increased GVHD mortality post-BMT in comparison to isotype control (p<.01). Interestingly, use of IL-22 knockout (KO) donor marrow or T cells had no impact on survival or on the ability to clear A20 lymphoma post-BMT, but IL-22 KO BMT recipients demonstrated significantly increased mortality during GVHD (p<.01). The critical role of recipient-derived IL-22 was confirmed in a minor antigen-mismatched LP into B6 BMT model (Figure 1). IL-22 KO recipients again demonstrated significantly increased mortality during GVHD (p<.001) and histopathologic evidence of GVHD in the small (p<.01) and large (p<.001) intestine and liver (p<.001). Furthermore, BMT into hematopoietic IL-22 KO chimeras also demonstrated increased GVHD mortality (p<.05) and clinical scoring (p<.001), indicating that the source of protective IL-22 is residual host-derived radio-resistant hematopoietic cells.
In summary, IL-22 is produced post-BMT by host ILC that are eliminated during GVHD, and IL-22 deficiency increases GVHD morbidity and mortality. While IL-22 deficiency did not significantly alter the donor immune response, it did lead to increased GVHD pathology, loss of epithelial integrity, and damage to the ISC niche. IL-22 is thus critical for protection of host epithelium during GVHD but is not involved in GVL. This may be exploited in the future to reduce clinical GVHD without limiting the curative potential of the transplant.
Fouser:Pfizer: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal