Abstract
Abstract 3080
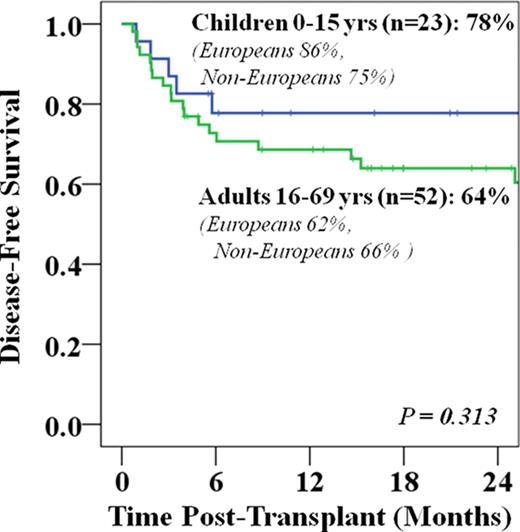
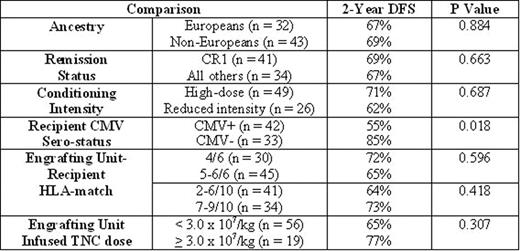
As compared to single-unit CBT, DCBT may improve engraftment and protect against relapse. Therefore, we have adopted DCBT for both children and adults with acute leukemia, myelodysplasia (MDS), and myeloproliferative diseases (MPD). However, determinants of disease-free survival (DFS) have yet to be fully established. Furthermore, whether DFS after DCBT is comparable in patients of European and non-European ancestry is of special interest. Therefore, we analyzed the DFS of 75 DCBT recipients with acute leukemia in morphologic remission or aplasia (n = 69), and MDS/MPD with ≤ 5% blasts (n = 6) transplanted from 10/2005-4/2011. Nearly all patients had high-risk disease. Children 0–15 years (n = 23) had the following characteristics: median age 9 years (range 0.9–15); median weight 37 kg (range 7–72); 30% European; and 26% CMV sero-positive. Diagnoses were 43% AML (or biphenotypic), 52% ALL, and 4% MDS/MPD, and all received high-dose conditioning. The children received grafts with a median infused TNC × 107/kg of 3.3 (larger unit) and 2.6 (smaller unit), and 2% of units were 6/6 HLA-A, -B antigen, -DRB1 allele matched, 63% 5/6, and 35% 4/6. Adults ≥ 16 years (n = 52) had the following characteristics: median age 41 years (range 16–69); median weight 69 kg (range 47–105); 48% European; 69% CMV sero-positive; and diagnoses were 63% AML (or biphenotypic), 27% ALL, and 10% MDS/MPD. Fifty percent received high-dose and 50% reduced intensity conditioning. Their units had a median infused TNC/kg of 2.7 and 1.9, and 3% were 6/6 HLA-matched, 47% 5/6, and 50% 4/6. All patients (pediatric and adult) received calcineurin-inhibitor/ mycophenolate mofetil immunosuppression, and none received anti-thymocyte globulin. Sustained donor neutrophil engraftment was seen in 91% of children and 94% of adults at medians of 20 and 26 days, respectively. The incidence of grade II-IV acute GVHD by day 180 was 44% in children and 58% in adults. Day 100 transplant-related mortality (TRM) was 9% in children and 19% in adults. The 2-year relapse incidence was 9% in children and 6% in adults. With a median follow-up of survivors of 26 months (range 4–70), 2-year Kaplan-Meier estimate of DFS was 78% in children and 64% in adults (Figure). Differences in survival by age did not reach significance. Univariate analysis of variables potentially influencing 2-year DFS (with log rank estimates of significance) in all patients is shown in the Table. There were no differences in 2-year DFS according to ancestry, remission status, and conditioning intensity. There was also no difference in 2-year DFS according to engrafting unit-recipient HLA-match (4-6/6 or 10 allele), or engrafting unit infused TNC dose/kg. However, patients who were CMV seronegative had a higher 2-year DFS (85% vs 55%, p = 0.018). Multivariate analysis revealed recipient CMV serostatus was a predictor of DFS independent of patient age, and its effect was mediated by an influence on TRM. We have previously shown that DCBT extends transplant access to minority patients. We now demonstrate that DCBT can achieve high and comparable DFS in both European and non-European pediatric and adult patients with acute leukemia and MDS/MPD. While these are very encouraging results further investigation in racial/ethnic sub-groups is needed. Nonetheless, our findings support DCBT as an immediate alternative therapy for high-risk acute leukemia in patients without suitable unrelated volunteer donors, especially given the very low incidence of relapse.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal