Abstract
Abstract 2678
Diffuse large B-cell lymphoma (DLBCL) is a heterogeneous disease characterized by a wide range of clinical outcomes. Rituximab added to CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) chemotherapy, R-CHOP has made a marked improvement in outcome in patients with DLBCL. The International Prognostic Index (IPI), which consists of age > 60 years, stage III/IV, elevated lactate dehydrogenase (LDH) level, Eastern Cooperative Oncology Group (ECOG) performance status (PS) † 2, and more than one extranodal (EN) site of disease, remains the most commonly used system for risk classification in DLBCL. However, recent studies suggested that new agent has altered the significance of previously recognized risk factors. Here we investigate the prognostic impact of reported risk factors in a large DLBCL patient cohort in a single institute to determine a better prognostic model in rituximab era.
In total, 250 newly diagnosed DLBCL patients treated with R-CHOP regimen at the Cancer Institute Hospital of JFCR between October 2003 and December 2008 were included and analyzed. Progression free survival (PFS) and overall survival (OS) were estimated using the Kaplan-Meier method and compared among risk groups using the log rank test. The Cox proportional hazards model was used to test the significance of prognostic factors. ROC curve was used to determine optimal serum level of sIL-2R and LDH as a cut off value for 4-year mortality risk.
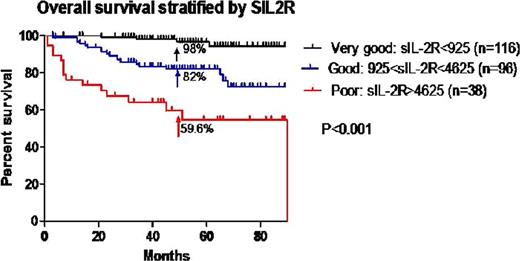
The median age of patients was 65 years (range 23–88 years), 56% were male. The median follow-up time was 49 months (range 1–90 months) and 39 deaths had been recorded by the time of the last follow-up. The IPI still remains predictive with an OS ranging from 52.4% to 91.6% at 4 years; however it cannot discriminate between low and low-intermediate group. Revised IPI was valid as well with an OS ranging from 63.3% to 97%. In univariate analysis, elevated sIL-2R level, B symptom, elevated LDH level, PS>2, age>65, stage III/IV, CD5 positive, and EN>1 were significant as poor prognostic factors whereas sex, bulky mass, MIB1 index >90%, Non-GCB were not. Furthermore, multivariate analysis showed that only sIL-2R>924U/ml, CD5 expression, and EN>1 were significant with relative hazard 1.4∼17.5, 1.4∼8.9, and 1.3∼4.7, respectively. As elevated sIL-2R was the most powerful prognostic factor, we performed further analysis on this parameter. Average serum sIL-2R level was 2,775U/ml (range from 220U/ml to 43,100U/ml) with a normal limit of upper is 230U/ml. ROC curve demonstrated that serum sIL-2R was more optimal value than serum LDH to identify high risk patients for 4-year mortality after initiation of R-CHOP therapy and cutoff value of sIL-2R was 924U/ml (1.73 upper limit of normal). sIL-2R level can be divided into three distinctprognostic groups. Patients with sIL-2R<925U/ml fall into a very good group with a 4-year OS:98% and 4-year PFS:90.7%, patients with 925U/ml<=sIL-2R<4,625U/mlfall into a good group with a 4-year OS:82% and 4-year PFS:77.7%, and patients with sIL-2R>=4,625U/ml fall into a poor group with a 4-year OS:59.6% and 4-year PFS:54.7% (P < 0.001).
sIL-2R level is an independent and powerful prognostic factor in serum level dependent manner in DLBCL patients treated with R-CHOP. This prognostic model should be reassessed on a larger scale and prospective study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal