Abstract
Abstract 2176
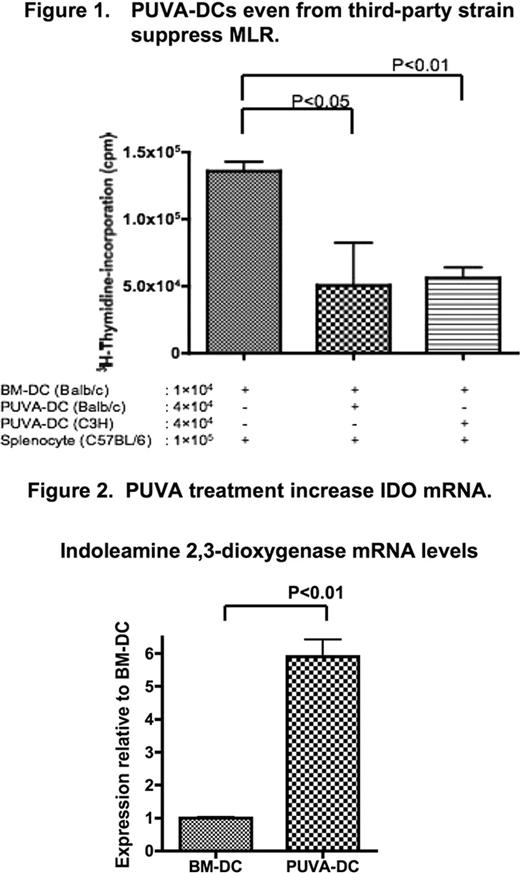
Extracorporeal photopheresis (ECP) is a leukapheresis-based immunomodulatory therapy by exposing isolated white blood cells to photoactive 8-MOP (psoralen) and UVA radiation (PUVA) for refractory acute and chronic graft-versus-host disease (GVHD). Although the effects of PUVA treatment on immune system remain poorly characterized, we have reported that bone marrow-derived dendritic cells (BM-DCs), which are generated from bone marrow cells plus GM-CSF, acquired tolerogenicity by PUVA-treatment in mice. In mixed lymphocyte reaction (MLR) assays, strong tolerogenicity was observed when adding PUVA-DCs generated from the same strain of stimulator cells, or responder cells, or even from third-party (Figure 1) strain into MLR mixture. That is, the PUVA-treated DCs have tolerogenic function in a MHC-independent manner (52nd ASH), in part, due to the reduced expression levels of CD80 and CD86, both of which are costimulatory molecules for T cell activation. To clarify the mechanisms of how PUVA-treated DCs induce tolerogenicity in further detail, we performed MLR with the addition of neutralizing antibodies against IL-10 or TGF-β1 or both, which have immunosuppressive effects. Neutralization of immunosuppressive cytokines had no effects on MLR. We then hypothesized that cell-to-cell contact between PUVA-DCs and alloreactive T-cells was needed to mediate the regulatory effect. To this end, we performed MLR using transwell to prevent cell-to cell contact. MLR was not suppressed when transwell was used, suggesting that PUVA-DCs dominantly regulates the alloreaction in a cell contact-dependent manner. Next we compared the expression of the indoleamine 2,3-dioxygenase (IDO), which induces T-cell anergy by tryptophan depletion and by the production of metabolic byproducts collectively known as kynurenines, by real-time PCR between PUVA-DCs and BM-DCs. An increased IDO gene transcription level was observed in PUVA-DCs about 5 times more than in BM-DCs (p<0.01) as shown in Figure 2. This suggested that the PUVA-treated DCs induced tolerogenic function by depleting tryptophan in the immediate environment. The question we have to consider next is whether tolerogenic capacity is acquired only in DCs or other lymphocytes subpopulations, because recent rodent studies have shown that the transfer splenocytes treated with PUVA prevent GVHD. To test this, PUVA-treated CD4, CD8, and B220 cells from the same strain of stimulator cells were added into the MLR mixture. MLR was suppressed only when PUVA-DCs were added. In conclusion, PUVA-DCs, but not other lymphocytes subpopulations, acquired regulatory function in a MHC-independent manner by upregulation of IDO. Infusion of PUVA-treated DCs could have a great potential to treat lethal acute GVHD in clinical settings.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal