Abstract
Abstract 2132
Studies have provided conflicting evidence on the etiology of hypogonadism in patients with sickle cell disease. A cross-sectional study was conducted on adult men with SCD to determine whether hypogonadism in these patients is due to primary testicular failure or secondary pituitary / hypothalamic dysfunction and to look for association between hypogonadism and serum ferritin levels. The study protocol was approved by Wayne State University / Detroit Medical Center Human investigation committee.
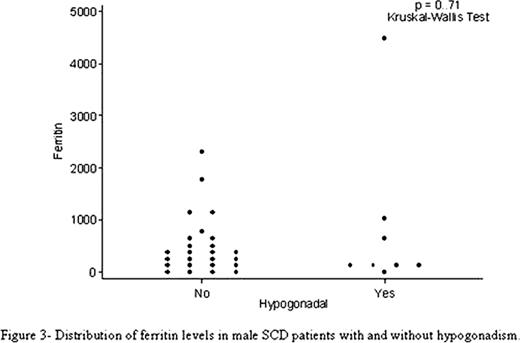
A total of 19 male patients with SCD 18 years or older following at the benign hematology clinic of Detroit Medical Center between Sep 21 to Dec 21; 2011 consented to participate in the study. Blood sample was drawn between 9AM – 11 AM and sent to the laboratory for hormonal assay. A previous pilot study (completed few months earlier) of 15 adult male patients with SCD aged 18years or older at the same site was also included in the analysis. The pilot study was approved by Wayne State University / Detroit Medical Center Human investigation committee. Serum samples from 15 patients with sickle cell disease who had blood work during their routine clinic visit at the benign hematology clinic was assessed for testosterone, FSH and LH levels. Thus a total of 34 male patients with SCD were included in the final analysis. Hormone measurements were done for total testosterone (using immunoassay), FSH and LH using two site sandwich immunoassay by chemilumino method (Siemens, Centaur XP). Additional information on body mass index (BMI), hemoglobin, total bilirubin, ferritin and creatinine levels was collected from the Electronic Medical Record (EMR).
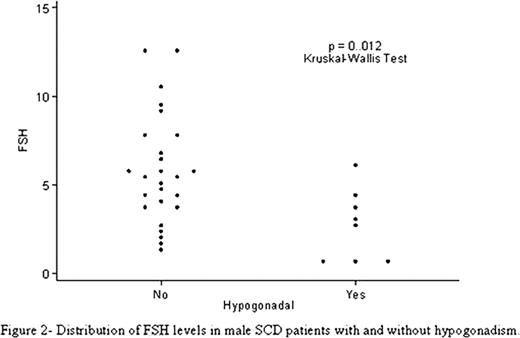
Hypogonadism was defined as serum total testosterone level of ≤250 ng/dL. Hypogonadal patients with high FSH and LH were considered as having primary/peripheral hypogonadism where as those with low FSH and LH or inappropriately normal (normal FSH and LH despite low serum testosterone) were considered to have secondary/central hypogonadism. FSH level between 1.5–12.4mIU/ml and LH level of 2–14mIU/ml was considered as normal for male adults. Stata 11.1 was used for statistical analysis. Kruskal-Wallis tests were used to assess the statistical significance of differences in hormone and ferritin levels; no adjustment was made for multiple comparisons.
Our study provides evidence for a central etiology to hypogonadism in male patients with SCD. In this small study ferritin level was not significantly related to hypogonadism.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal