Abstract
Abstract 2049
Post-transplant thrombocytopenia is universal among recipients of hematopoietic stem cell transplantation (HSCT). We have previously reported a secondary post-transplant thrombocytopenia following autologous HSCT which is associated with poor survival (Ninan MJ, et al., BBMT 2007), however the clinical significance of a fall post-engraftment in platelet counts among recipients of allogeneic HSCT has not been studied.
A total of 929 consecutive pts who underwent allogeneic HSCT between 1993 and 2009 were studied in an IRB-approved retrospective analysis. 55% of pts were male and 45% were female with a median age of 43 ± 12.6 years. Diagnoses included: acute leukemia (423, 46%), chronic leukemia (197, 21%), non-Hodgkin's lymphoma (110, 12%),myelodysplastic syndrome (93, 10%), multiple myeloma (26, 3%), and other less common malignancies (80, 8%). Disease status was classified into five different categories: complete remission (287, 31%), partial remission (297, 34%), refractory (180, 19%), untreated (28, 3%) and incompletely classified (137, 15%). Grafts were obtained from related donors in 595 pts (64%), and unrelated donors in 334 pts (36%), with 55% peripheral blood stem cell (PBSC), 42% bone marrow (BM), and 3% cord blood units or multiple sources. Blood platelet counts and platelet transfusions were collected from 15 days pre-transplant until 100 days post-transplant. Platelet engraftment was defined as a platelet count ≥ 50 x10E3/mcL without a platelet transfusion in the previous 7 days. Pts (n=816) who achieved platelet engraftment and survived at least 30 days were selected for further analysis.
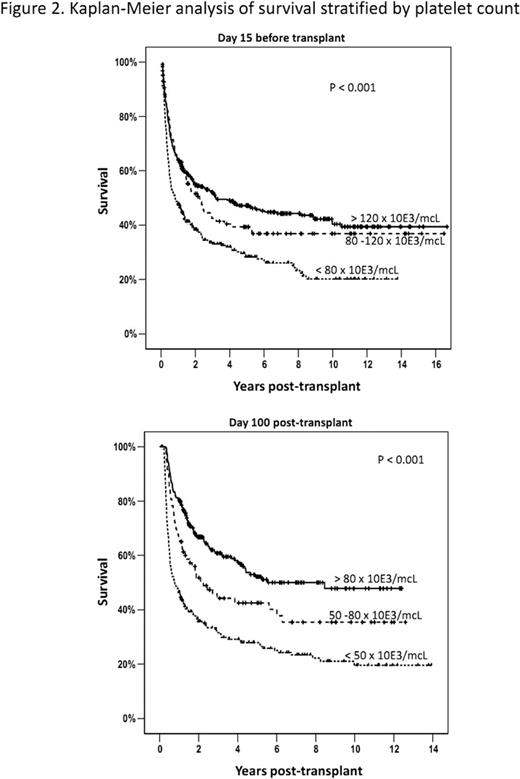
The 816 evaluable pts were divided into cohorts based upon their post-transplant survival: 146(18%) who died within 100 days post-transplant (early death); 267 (33%) that survived 100 days −2 years post-transplant (late death), 319 (39%) who survived > 2 years (long-term survival), and 84 (10%) were lost of follow-up within the first 2 years. Transfusion-independent platelet engraftment was achieved at median of 15 days post-transplant with no significant differences seen in the kinetics of initial engraftment among the different pt cohorts. Median platelet counts at different time points post-transplant were plotted for each pt cohort (Figure 1). Pts in the early-death cohort had a continuous decline in median platelet counts from engraftment values of > 50 x10E3/mcL to a median values of ∼20 x10E3/mcL. Univariate analyses indicated that higher platelet counts at day −15 (prior to conditioning) or at day 100 post-transplant were significantly associated with improved overall survival (HR of 0.63 and 0.39 respectively, P < 0.01). Cox-regression analysis was performed to evaluate significance of pre- and post-transplant platelet counts with clinical covariates that have been previously associated with survival including age, diagnosis, disease status and the source of the grafts. The multivariate model confirmed the significant association of the following factors with overall survival: higher platelet counts on day 15 pre-transplant (HR:0.81; 95%Cl:0.70∼0.93; P-value <0.01), the platelet count on day 100 post-transplant (HR: 0.62; 95%Cl:0.55∼0.70; P-value:<0.01 ), a diagnosis of acute leukemia (HR:1.64; 95%Cl:1.13∼2.39; P-value <0.01), a diagnosis of multiple myeloma (HR: 2.12; 95%Cl:1.05∼4.23; P-value= 0.04), a disease status of complete remission (CR) versus not in CR (HR: 0.66; 95%Cl:0.44∼0.97; P-value = 0.04), and age (HR: 1.01; 95%Cl:1.00∼1.02; P-value= 0.08). Kaplan-Meier estimates for survival were performed based upon stratification of pt groups on the platelet count at day-15 pre-transplant or the day +100 post-transplant platelet count (Figure 2). Pts with a platelet count > 80 × 10E3/mcL on day +100 had 5 year survival of more than 50% compared with 30% survival in the pt cohort with platelet counts < 50 x10E3/mcL on day +100.
Pts with continuously low platelet count after initial platelet engraftment are at high risk for early death. Higher pre-transplant platelet may be a surrogate for disease status and extent of prior therapy and are associated with long-term survival among pts undergoing allogeneic HSCT. Post-transplant thrombopoiesis at day 100 is highly correlated with long-term survival after allogeneic HSCT, identifying a high-risk group of transplant pts for whom additional treatment strategies are needed.
Gleason:Celgene, Merck, Millenium: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal