Abstract
Abstract 2013
Allogeneic stem cell transplantation (ASCT) with T-cell depleted (TCD) allograft has been used to decrease the risk of graft-versus-host disease (GVHD). How outcomes of ASCT with TCD grafts compares to transplant with unmodified grafts in the context of ablative, reduced toxicity conditioning with busulfan /fludarabine is unknown. We sought to compare ASCT with and without TCD grafts, by studying the outcomes of pts with acute myeloid leukemia (AML) in first complete remission (CR1) who had TCD allografts at Memorial Sloan Kettering Cancer Center (MSKCC) with those who had unmodified allografts at MD Anderson Cancer Center (MDACC).
Transplants at MSKCC (N=115) and MDACC (N=181) were performed between 2001 and 2010. Preparative regimens at MSKCC included: 1) Hyperfractionated total body irradiation (HFTBI) 1375 cGy over 4 days, thiotepa 5 mg/kg/day × 2 days & fludarabine 25 mg/m2/day × 5 days (n=29); 2) HFTBI 1375 cGy over 4 days, thiotepa 5 mg/kg/day × 2 days & cyclophosphamide 60 mg/kg/day × 2 days (n=25); or 3) busulfan 0.8 mg/kg intravenously every 6 hours for 10 doses(n=42) or 12 doses (n=19), melphalan 70 mg/m2/day × 2 days & fludarabine 25 mg/m2/day × 5 days (total n=61). Peripheral blood (PB) grafts underwent CD34+ cell selection using the ISOLEX 300i system, followed by sheep red blood cell (sRBC)-rosette depletion (n=85); or CD34+ cell selection using the CliniMACS system alone (n=22). Bone marrow (BM) grafts were T cell depleted by sequential soybean lectin agglutination and sRBC-rosette depletion (n=8). No additional GVHD prophylaxis was administered at MSKCC.
Fludarabine 40 mg/m2 and busulfan 130 mg/m2 intravenously once daily for 4 days were used for conditioning at MDACC, with tacrolimus and mini-methotrexate for GVHD prophylaxis. Pts with unrelated or HLA-mismatched donors treated at MDACC and MSKCC received equine (total 60 mg/kg) or rabbit (total 2.5–5 mg/kg) anti-thymocyte globulin. Cytogenetic risk stratification considered complex cytogenetics, -5, -5q, -7, -7q, 11q23 aberrations, inv(3), t(3;3), t(6;9), and t(9;22) as poor risk.
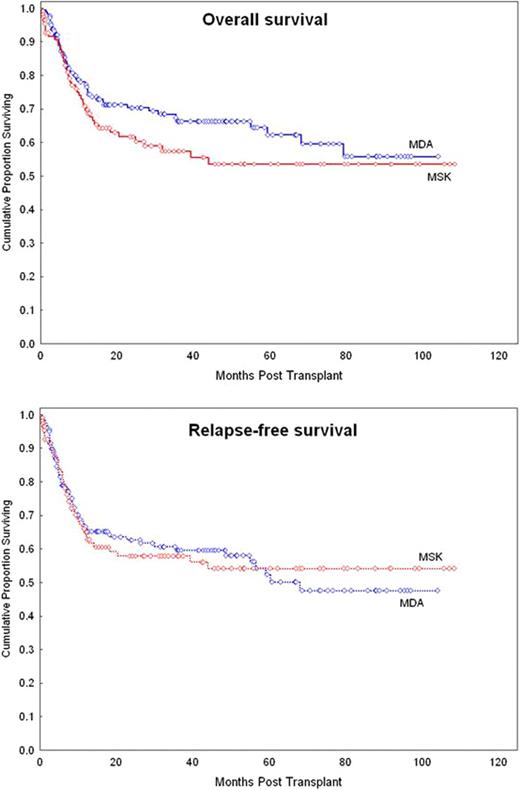
Pt characteristics and outcomes are summarized in the Table. TCD recipients were more likely to be older, receive a mismatch transplant, and have PBSC used as a graft source. Overall, only one pt, who had received an unmodified graft, experienced primary graft failure. Eleven (10%) and 33 (18%) pts experienced grade ≥2 acute GVHD within 100 days after transplants with TCD and unmodified grafts, respectively (p=0.05). Three-year relapse-free and overall survival rates were 58% and 57% in pts who received TCD grafts, and 60% and 66% in pts who received unmodified grafts (P=NS; Figure). There was a trend towards lower early non-relapse mortality among pts who received unmodified grafts (3% vs. 8% at 100 days, p=0.07). Of age, sex, secondary disease, risk status, donor, and graft type, secondary AML was the only risk factor found to significantly influence overall survival (HR: 1.7, 95% CI: 1.1–2.8). Survival outcomes were still comparable between recipients of TCD and unmodified grafts after adjusting for secondary AML. None of these factors significantly predicted relapse-free survival.
Myeloablative ASCT with TCD or unmodified allografts lead to comparable outcomes in this high-risk cohort of AML pts in CR1 with a lower acute GVHD rate observed after TCD transplants.
| Characteristics . | Frequency, n (%) . | ||
|---|---|---|---|
| . | TCD, N=115 . | Unmodified, N=181 . | p . |
| Time CR1 to transplant, days* | 83 (12–304) | 97 (8–455) | 0.040 |
| Age, years* | 52 (19–71) | 48 (18–63) | <0.001 |
| >50 years | 66 (57) | 76 (42) | 0.010 |
| Sex = Female | 58 (50) | 90 (50) | NS |
| Etiology | |||
| de novo | 60 (52) | 144 (80) | <0.001 |
| Secondary | 38 (33) | 24 (13) | |
| Therapy-related | 17 (15) | 13 (7) | |
| Cytogenetic risk status | NS | ||
| Good | 1 (1) | 2 (1) | |
| Intermediate | 72 (63) | 103 (57) | |
| Poor | 42 (37) | 76 (42) | |
| Donor type | |||
| MRD | 56 (49) | 103 (57) | |
| MUD | 32 (28) | 64 (35) | |
| MM | 27 (23) | 14 (8) | <0.001 |
| Graft type | |||
| BM | 8 (7) | 57 (32) | <0.001 |
| PB | 107 (93) | 124 (68) | |
| Outcome (95% CI) | |||
| 3-year RI | 18% (12%–27%) | 25% (19%–33%) | NS |
| 100 day NRM | 8% (4%–15%) | 3% (1%–7%) | 0.07 |
| 1-year NRM | 18% (12%–27%) | 13% (9%–19%) | NS |
| 3-year NRM | 24% (17%–34%) | 16% (11%–23%) | NS |
| 3-year RFS | 58% (47%–67%) | 60% (51%–67%) | NS |
| 3-year OS | 57% (47%–67%) | 66% (58%–74%) | NS |
| Characteristics . | Frequency, n (%) . | ||
|---|---|---|---|
| . | TCD, N=115 . | Unmodified, N=181 . | p . |
| Time CR1 to transplant, days* | 83 (12–304) | 97 (8–455) | 0.040 |
| Age, years* | 52 (19–71) | 48 (18–63) | <0.001 |
| >50 years | 66 (57) | 76 (42) | 0.010 |
| Sex = Female | 58 (50) | 90 (50) | NS |
| Etiology | |||
| de novo | 60 (52) | 144 (80) | <0.001 |
| Secondary | 38 (33) | 24 (13) | |
| Therapy-related | 17 (15) | 13 (7) | |
| Cytogenetic risk status | NS | ||
| Good | 1 (1) | 2 (1) | |
| Intermediate | 72 (63) | 103 (57) | |
| Poor | 42 (37) | 76 (42) | |
| Donor type | |||
| MRD | 56 (49) | 103 (57) | |
| MUD | 32 (28) | 64 (35) | |
| MM | 27 (23) | 14 (8) | <0.001 |
| Graft type | |||
| BM | 8 (7) | 57 (32) | <0.001 |
| PB | 107 (93) | 124 (68) | |
| Outcome (95% CI) | |||
| 3-year RI | 18% (12%–27%) | 25% (19%–33%) | NS |
| 100 day NRM | 8% (4%–15%) | 3% (1%–7%) | 0.07 |
| 1-year NRM | 18% (12%–27%) | 13% (9%–19%) | NS |
| 3-year NRM | 24% (17%–34%) | 16% (11%–23%) | NS |
| 3-year RFS | 58% (47%–67%) | 60% (51%–67%) | NS |
| 3-year OS | 57% (47%–67%) | 66% (58%–74%) | NS |
: Median (range).
TCD: T-cell depleted, CR1: First complete remission, MRD: Matched related donor, MUD: Matched unrelated donor, MM: HLA-mismatch donor, BM: Bone marrow, PB: Peripheral blood, RI: Relapse incidence, NRM: Non-relapse mortality, RFS: Relapse-free survival, OS: Overall survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal