Abstract
Abstract 2012
High dose chemotherapy (HDC) followed by autologous stem cell transplant (ASCT) remains a valid treatment option for patients with multiple myeloma (MM). HDC has improved response rate, event-free survival (EFS) and treatment free interval for patients with MM when compared with conventional chemotherapy. To date, Melphalan 200 mg/m2 (HDM) remains the standard ASCT preparative regimen as no other regimens have demonstrated improved outcomes with acceptable toxicity. Nevertheless, relapse remains inevitable with this approach prompting continued search for better therapies. To overcome resistance and early relapse we used a more aggressive alkylator based conditioning regimen. Here we summarize a retrospective study of the long-term follow-up of newly diagnosed MM patients treated with the preparative regimen Carmustine, 500 mg/m2 and Melphalan, 200 mg/m2 (BCNU/HDM) followed by ASCT versus a subsequent group of patients treated with HDM alone and ASCT.
Between November of 1997 and December of 2008, 207 patients with MM underwent HDC followed by ASCT at our Institution, using either BCNU/HDM (n = 104, treated between 1997–2002) or HDM (n = 103, treated between 2002–2008) as the preparative regimen. Presenting patient characteristics were similar (age, gender, MM type, hemoglobin, creatinine, calcium, plasma cell infiltration, Durie-Salmon stage, and ISS stage). Patients treated with BCNU/HDM were diagnosed preceding the introduction of novel anti-MM agents such as thalidomide, lenalidomide, and bortezomib and thus did not receive these as induction therapy, while HDM patients received various combinations of novel agents as induction therapy.
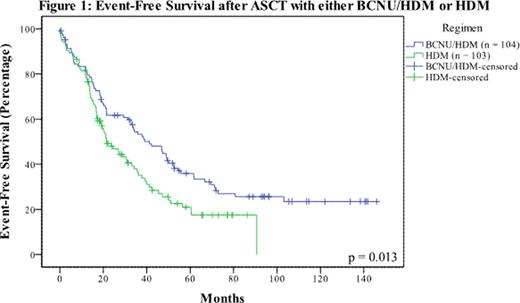
With a median follow-up for surviving patients of 96 and 34 months for the BCNU/HDM and HDM cohorts, respectively, the event-free survival (EFS) was significantly increased with the BCNU/HDM conditioning regimen (41.7 months) as compared with the HDM regimen (21.6 months, p = 0.013) (Figure 1). Median overall survival (OS) was 83.1 months with BCNU/HDM vs. 68.2 months with HDM (p = 0.359 at current follow-up) with 34% of BCNU/HDM patients alive at >10 years (Figure 2). In the BCNU/HDM group, 47/104 patients achieved ≥VGPR and this subgroup had a median OS of 103 months. Nineteen patients in the BCNU/HDM group are ≥7 years from ASCT and 18 (17%) have never required treatment for progressive disease. Engraftment and transplant-related mortality were similar in both groups (3% TRM in the BCNU/HDM and 4% TRM in the HDM arm). The BCNU/HDM group had a higher incidence of pneumonitis (50%) vs. the HDM group (15%) but this was managed with short courses of steroids and was never fatal. Focusing on the subgroup of patients who proceeded to transplant immediately after only 1 induction course, the median OS was 103 months for the BCNU (80 patients) containing arm versus 69 months for the HDM (71 patients) arm (p=0.085), suggesting a clear trend further favoring this dose dense approach.
EFS was superior with the BCNU/HDM regimen compared with HDM and a subgroup of patients treated with BCNU/HDM have achieved EFS >7 years without any additional therapy. Engraftment and treatment related mortality were similar in both groups despite advances in supportive care for the HDM group. Our findings suggest that BCNU/HDM should be compared in a randomized prospective fashion to HDM as an ASCT preparative regimen following optimal induction therapy with novel agents to determine whether this will lead to further improvements in EFS and OS following ASCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal