Abstract
Abstract 1736
The distinction between Acute Myeloid Leukaemia (AML) and Myelodysplastic Syndrome (MDS), together with its prognostic assessment, depends on the proportion of bone marrow blast cells. The International Prognostic Scoring System (IPSS) uses this value to predict survival in conjunction with cytogenetic and blood count parameters. Current practice in most centres is to count blast cells manually on stained smears and to assign patients to one of 4 bands (<5%, 6–10%,11-19% and >20%). This approach has two major disadvantages. Firstly, the evaluation of cellular morphology is subjective and the standard error of a manual count is sufficiently large that many patients cannot be assigned with reasonable accuracy to a category - which can critically impact on their care. Secondly, assigning patients into broad groups, instead of retaining blast cell count as a continuous variable, may be degrading important prognostic information.
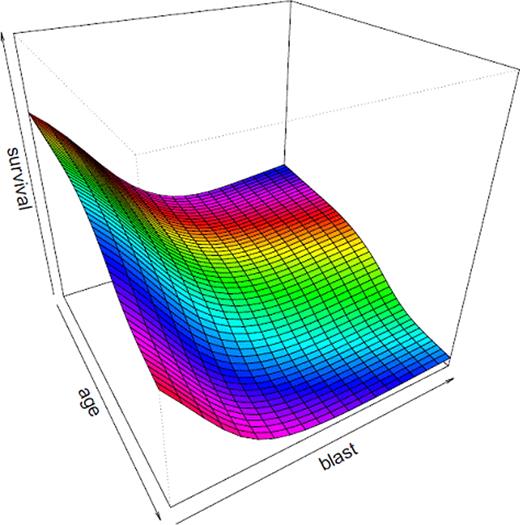
Modern flow cytometric techniques allow blast cells to be counted with high levels of accuracy. In this study we used a standard five colour assay including CD34, CD117, CD15, CD3, CD19 and physical characteristics to count bone marrow blast cells. Bone marrows from 271 patients with AML/MDS treated with curative intent (median age, 59 yrs; M: F,1.22) and 684 patients treated with supportive therapy (median age, 77 yrs; M: F,1: 1.8) were evaluated. Patients with acute promyelocytic leukaemia (APML), AML with t(8;21) or inv 16 were excluded. All patients were from a population-based cohort (www.hmrn.org), and all diagnostic studies were performed using standard protocols in a single laboratory. A prognostic model was constructed using age, flow cytometric blast cell count and gender. In non-intensively treated patients survival declined rapidly with blast counts up to 10% and then decreases much more slowly. Age had a minimal effect on survival under the age of 70, but prognosis declined rapidly in older patients. Male gender was a significant adverse risk factor (hazard ratio = 1.47). In contrast, patients who were treated intensively showed only a modest relationship between blast count and prognosis but a much more marked effect of age. Survival declined progressively from 20 years with the trend accelerating in those over 60 years. There was also a smaller effect of gender in those receiving intensive treatment (hazard ratio = 1.09). In MDS patients, a complex relationship between blast cell count, standard cytogenetic risk factors and the degree of cytopenia was observed.
Using age and flow cytometric blast count as continuous variables, modelled using restricted cubic splines, together with gender enabled more accurate outcome prediction in patients with AML and MDS across the full range of blast counts. This is possible because of the much higher levels of accuracy of flow cytometry compared to manual counting methods. The main practical advantage of a unified prognostic model is that it allows the relative benefits of intensive and non-intensive treatment to be readily compared for an individual patient. The predictive power of this core model can be improved further by the inclusion of additional clinical and molecular data. MDS and most forms of AML are part of a continuous spectrum of disease. A more unified approach to classification avoiding arbitrary subdivision may improve clinical decision making in this complex group of patients.
The interrelationship between survival, age and blast cell count in patients with myelodysplastic syndrome.
The interrelationship between survival, age and blast cell count in patients with myelodysplastic syndrome.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal