Abstract
Abstract 1720
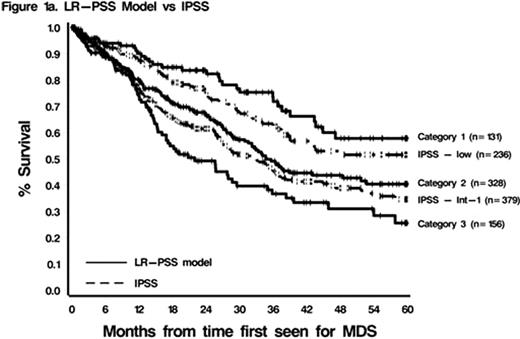
The myelodysplastic syndromes are commonly divided into lower- and higher-risk subtypes depending on blast percentage and International Prognostic Scoring System (IPSS) score (0–1.0, low or Int-1, median overall survival (OS) 3.5–5.7 years). Because the IPSS is limited in its ability to identify poor prognosis lower-risk patients (pts), a prognostic scoring system specifically for lower-risk MDS pts (LR-PSS) was developed (Garcia-Manero Leukemia 2008) at MD Anderson (MDA), based on unfavorable (non-del(5q), non–diploid) cytogenetics, hemoglobin (hgb) <10g/dl, platelet count (plt) <50 k/uL or 50–200k/uL, bone marrow blast %≥4, and age ≥60 years. The IPSS-R (Greenberg Leuk Res 2011) improves upon the IPSS using novel cytogenetics classifications (Schanz EHA 2010) and a neutrophil cut-off of 800 k/uL. We validated the LR-PSS and the IPSS-R in a separate cohort of lower-risk MDS patients seen at Cleveland Clinic (CC) or at MDA not included in LR-PSS development.
Of 1293 MDS patients identified at CC or MDA from 1991–2010, 664 had lower-risk disease and adequate data for analyses. OS was calculated from first date seen at either institution. The Kaplan–Meier method was used to estimate median OS. Univariable analyses were performed using the log-rank test; multivariable analyses used a Cox proportional hazards model stratified by treatment center. Harrell's c index and the Akaike information criteria (AIC) were used to assess the discriminatory power of the models and relative goodness of fit, respectively.
Comparing CC to MDA, baseline values were similar except median age: 70 vs. 67 years (p=.02); time since diagnosis: 2.7 vs. 1.1 months (p<.0001); hgb <10: 51% vs. 43% (p=.05); plt <50k/uL: 30 vs. 24% (p=.06); ANC <1.5 k/uL: 27% vs. 36% (p=.01); blasts <4%: 75% vs. 65% (p=.003); WHO classification RA/RARS/RCMD/CMML: 11/15/26/12% vs. 16/9/45/0% (p<.0001). Cytogenetics were diploid: 61% vs. 66%; del(5q): 9% vs. 2%; del(20q): 3% vs. 5%; -Y: 4% vs. 2%, respectively (p=.5). Median OS was 36.8 months (95% C.I. 33–45) and median follow-up of patients still alive was 13.9 months (range 0.01–155). LR-PSS and IPSS-R classifications for CC and MDA Pts and OS are in Table 1 and Figure 1. In univariable analyses, The IPSS, LR-PSS, and IPSS-R were all predictive of OS (p=.002, <.0001, and <.0001, respectively). Multivariable analyses confirmed the overall predictive abilities of the prognostic tools and of Hgb, plt, age, and IPSS/IPSS-R cytogenetics (all p≤.03). Compared to the IPSS-R, the LR-PSS had the higher (better) Harrell's c value (.64 vs.63) and lower (better) AIC (2518 vs. 2525). The LR-PSS upstaged 156 pts (25%) from IPSS low or Int-1 to LR-PSS Category 3, and downstaged 47 pts (12%) from Int-1 to Category 1. The IPSS-R upstaged 164 pts (27%) from IPSS low or Int-1 to IPSS-R Categories ≥Intermediate, and downstaged 5 pts (1%) from Int-1 to Very Good.
LR-PSS and IPSS-R Survival Estimates
| LR-PSS Category: . | CC n = 292(%) . | MDA n = 372(%) . | Median Survival in Months, MDA 2008 (%) . | Median Survival in Months, CC + MDA (%) . |
|---|---|---|---|---|
| 1 | 52 (21) | 79 (21) | 80.3 (21) | 91.4 (21) |
| 2 | 139 (57) | 190 (51) | 26.6 (48) | 35.6 (53) |
| 3 | 53 (22) | 103 (28) | 14.2 (31) | 22.0 (25) |
| IPSS-R Category: | Median Survival in Months, IPSS-R | |||
| Very Good | 48 (20) | 64 (17) | 81.6 | 91.4 (18) |
| Good | 135 (56) | 202 (55) | 51.6 | 35.9 (55) |
| Intermediate | 47 (19) | 79 (21) | 27.6 | 27.8 (27)* |
| High | 11 (5) | 20 (5) | 18 | |
| Very High | 2 (1) | 5 (1) | 10.8 |
| LR-PSS Category: . | CC n = 292(%) . | MDA n = 372(%) . | Median Survival in Months, MDA 2008 (%) . | Median Survival in Months, CC + MDA (%) . |
|---|---|---|---|---|
| 1 | 52 (21) | 79 (21) | 80.3 (21) | 91.4 (21) |
| 2 | 139 (57) | 190 (51) | 26.6 (48) | 35.6 (53) |
| 3 | 53 (22) | 103 (28) | 14.2 (31) | 22.0 (25) |
| IPSS-R Category: | Median Survival in Months, IPSS-R | |||
| Very Good | 48 (20) | 64 (17) | 81.6 | 91.4 (18) |
| Good | 135 (56) | 202 (55) | 51.6 | 35.9 (55) |
| Intermediate | 47 (19) | 79 (21) | 27.6 | 27.8 (27)* |
| High | 11 (5) | 20 (5) | 18 | |
| Very High | 2 (1) | 5 (1) | 10.8 |
(Combined Intermediate + Good + Very Good)
The LR-PSS and IPSS-R are valid tools for distinguishing among pts previously thought to have lower-risk disease by the IPSS, and identifying those who have better and worse survival. This latter group of pts may benefit from earlier interventions with disease-modifying therapies, and should be considered in trials targeting higher-risk MDS pts. The LR-PSS appears to provide slightly better prognostic information.
Sekeres:Celgene: Consultancy, Honoraria, Speakers Bureau. Maciejewski:Celgene: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal