Abstract
Abstract 1610
As for the prognostic factors of elderly patients with diffuse large B-cell lymphoma (DLBCL) treated with R-CHOP, limited reports have been available. Although the maintenance of relative dose intensity (RDI) has been considered to improve the outcome, recent reports show that dose-reduced R-CHOP also has successful results on elderly DLBCL (Lancet Oncology. 2011; 12: 460). As rigid adherence to R-CHOP protocol is difficult in the treatment of elderly DLBCL, we investigated the relationship between RDI delivered and clinical outcomes in elderly patients with DLBCL.
We retrospectively analyzed a total of 109 consecutive DLBCL patients over 70 years who were diagnosed and received R-CHOP in our institution between January 2004 and January 2011. Among them, 56 % were male, and 38 % were over 80 years. 49 % of patients had an Ann Arbor stage III or IV, and ECOG performance status (PS) were >= 2 in 37 %. Lactate dehydrogenase (LDH) levels were higher than normal in 60 %. Age-adjusted IPI was 2–3 in 45 %. Charlson comorbidity index (CCI) was >= 2 in 23 %. Most patients with localized disease received 3 cycles of R-CHOP (delivered with 21-day interval) followed by radiation, and patients with advanced disease received 6 or 8 cycles of R-CHOP. In the first cycles of R-CHOP therapy, patients aged 70–79 years received 70 % dose of cyclophosphamide, adriamycin and vincristine. Patients over 80 years received 50 % dose of them. Predonisolone was also reduced to 40–60 mg on day 1–5 according to patients' condition. Thereafter, the doses were individually adjusted according to attending physicians' judgment. 78 % of the patients experienced grade 3–4 neutropenia and 21 % grade 3 febrile neutropenia. Two patients died of neutropenia and infection. 65 % of patients received prophylactic G-SCF. By using clinical records of these patients, we estimated the prognostic factors using the Cox regression model. Estimates of prognostic factors were expressed as hazard ratios (HR) and 95 % confidence interval (CI) based on the Cox regression. We did two-sided statistical tests, with a 5 % level of significance. This study was approved by our institutional review board.
After median follow up for living patients of 25.5 months, 41 deaths has occurred (including 22 due to lymphoma), and 2-year overall survival (OS) and progression-free survival (PFS) were 71.3 % [95 % CI 60.8 %–79.5 %] and 53.5 % [95 % CI 42.7
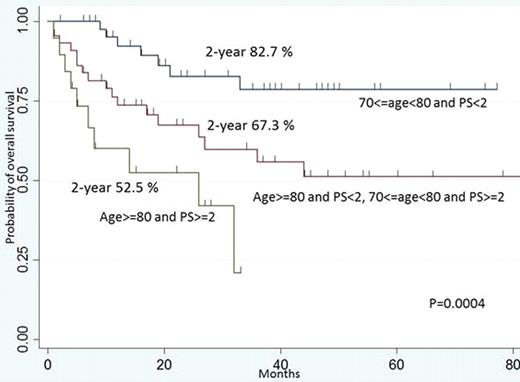
–63.1 %], respectively. Univariate and multivariate analysis revealed that LDH and staging at diagnosis were not associated with prognosis. PS >= 2 (HR 2.94, 95 % CI 1.48–5.84, P=0.002) and age >= 80 years (HR 2.05, 95 % CI 1.04–4.04, P=0.039) retained independent adverse prognostic values for 2-year OS in multivariate analysis. Dividing entire population into 3 groups using these 2 prognostic factors, 2-year OS were 82.7 % (70 <= age < 80 and PS < 2), 67.3 % (70 <= age < 80 and PS>=2 or age>=80 and PS < 2), and 52.5 % (age >= 80 and PS >= 2), respectively (log-rank, P=0.0004). Among the all 109 patients, 91 patients received >=3 cycles of R-CHOP and RDI could be calculated. RDI was strongly associated with age (R-squared 0.42, RDI (%) = 201-1.90x age (years)). When high age-adjusted RDI group (H-aaRDI) was defined as the group of patients who satisfied □eRDI > 201 - 1.90x age', and low age-adjusted RDI group (L-aaRDI) as □eRDI< 201 - 1.90x age', 2-year OS were equivalent between H-aaRDI and L-aaRDI groups (79.8 % vs 78.7 %, log-rank, P=0.36). When multivariate analysis was performed against those 91 patients, 2-year OS was also independently associated with PS >=2 (HR 3.12, 95 % CI 1.35–7.20, P=0.008) and age >=80 (HR 2.41, 95 % CI 1.04–5.59, P=0.041). Lower age-adjusted RDI did not have prognostic value (HR 1.28, 95 % CI 0.55 – 2.94, P=0.57).
Our retrospective analysis confirmed the efficacy of reduced-dose R-CHOP against elderly DLBCL, as was reported previously. Their prognosis was not associated with LDH level, staging, nor RDI delivered, but with ECOG PS and age over 80. Our findings indicated that strict adherence to keep RDI may not be necessary in the treatment of elderly DLBCL. The simple method to define optimal dose of R-CHOP for elderly should be explored.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal