Abstract
Dendritic cells (DCs) are antigen-presenting cells specialized to activate naïve T lymphocytes and initiate primary immune responses. The different classes of specific immune responses are driven by the biased development of pathogen-specific effector CD4+ T-cell subsets — that is, T helper 1 (Th1), Th2 and Th17 cells, that activate different components of cellular and humoral immunity. Th cell differentiation is critical for achieving proper immune responses, and imbalances in either the function or activity of these cell types are responsible for many immune diseases, including autoimmunity, cancer and allergy.
DCs reside in an immature state in many nonlymphoid tissues such as the skin, the intestine or airway mucosa which are under high exposure of pathogens and chemicals. DCs, which take up pathogens, develop their maturation processes, migrate to the T-cell areas of secondary lymphoid organs and interact with naïve T cells. TCR stimulation and co-stimulation allow naïve Th cells to develop into protective effector cells, normally accompanied by the high-level expression of selective sets of cytokines. The balance of these cytokines and the resulting class of immune response strongly depend on the conditions under which DCs are primed for the expression of the T-cell-polarizing molecules.
The ligands for many isoforms of toll-like receptors (TLRs), including certain nucleic acids, lipopolysaccharides (LPS) and fungus-derived glycoprotein molecules, alter the DC function, and induce Th1 differentiation in an antigen non-specific manner. In this process, IL-12 produced by DCs is clearly correlated with sensitization of Th1 lymphocytes in vitro and in vivo among the factors that have been shown to influence the Th1-Th2 balance.
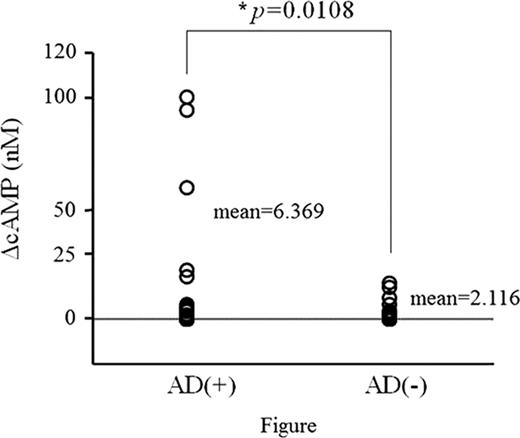
On the other hand, DCs matured in the presence of prostaglandin E2 (PGE2), histamine, or forskolin induce the differentiation of naïve CD4+ T cells toward Th2 via the cyclic adenosine 3',5'-monophosphate (cAMP) cascade. In vitro assay systems have been established to evaluate Th1/Th2 adjuvant activities, using MLR and intracellular cAMP concentration of antigen-presenting cells.
No relevant conflicts of interest to declare.

This icon denotes a clinically relevant abstract
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal