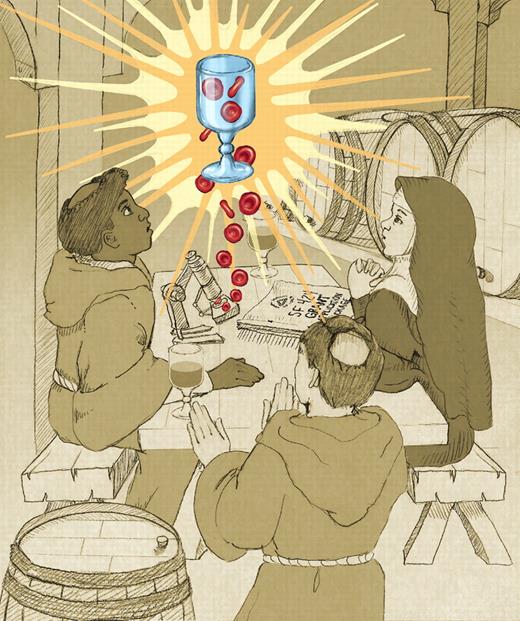
In this issue of Blood, Giarratana et al provide an important proof of principle in the quest for biotechnology's equivalent of the Holy Grail of blood transfusion: ex vivo manufacture of human red cells (RBCs) for therapeutic use (see figure).1
Red blood cells derived from culture (cRBCs) hold the promise of replacing an essential and widely used but relatively crude blood component with a standardized, well-characterized, readily available, unadulterated biologic manufactured under strictly controlled conditions. That is the dream. Several groups around the world have been able to generate erythroid cells on a laboratory scale from the hematopoietic progenitors (HSCs) in mobilized peripheral blood, bone marrow, and umbilical cord blood (UCB), and from embryonic stem cells (hESCs) and induced pluripotent stem cells (hiPSCs).2-5 Each “brewery” (or in this case winery?) has its own recipe. Most culture systems require a 3- or 4-step process to effect lineage-specific commitment, expansion, maturation, and enucleation, usually involving complex mixtures of growth factors and coculture with feeder cells, often of murine origin. The process takes 2 to 4 weeks. What the Paris group has achieved is production under Good Manufacturing Practice (GMP) conditions of a homogeneous population of autologous cells with the morphologic, biochemical, antigenic, and functional properties of RBCs, which in addition appear to store well at refrigerated temperatures and to circulate after transfusion with a half-survival time comparable with that of native RBCs. This represents the first transfusion in a human of cRBCs.
That is the good news. There are lots of caveats before we can anticipate replacing any of the estimated 90 million-plus units transfused worldwide with cRBCs. A standard unit of RBCs contains approximately 2.5 × 1012 RBCs, whereas the method described here required 13 L of culture medium to produce 1010 cRBCs, the result of a relatively modest cell amplification and enucleation rate. The reasons for this inefficiency are well known and in part result from the desire to produce an autologous product suitable for the transfusion phase of the study. However, scale-up remains a formidable hurdle. Proliferation can be improved some 10-fold using UCB progenitors as a starting material, and some investigators estimate that as many as 8 units of mature cRBCs could be generated from a single cord blood collection.6 Giarratana et al's cohort of synchronous cRBCs displays the characteristics of “stress reticulocytes,” not mature biconcave discs. This is novel in itself. The cells can mature into terminal discocytes in vivo.1 Such cells may eventually prove advantageous by increasing the transfusion interval, thus reducing iron accumulation in chronically transfused patients.7 However, these cells, judging from the single radiolabeling study, do not appear to circulate longer than do mature discoid RBCs; this finding may result from 51Cr labeling artifact, donor variability, culture conditions, or excessive cell handling. GMP will require methods to monitor cell quality and validate RBC potency and equivalence from lot to lot.8 Furthermore, differing culture conditions may modify the membrane remodeling process in a way that affects membrane protein organization and glycosylation and alters RBC immunogenicity. These are just some of the issues that must be addressed before clinical safety and efficacy trials can be undertaken.
With all of these caveats, this study still represents a significant step forward and a tribute to the long-standing international investment in the basic biology of hematopoiesis. The parallel advances in biotechnology that have led to the generation of clinical-grade growth factors and modern cell-culture methods have proved equally necessary for translating this basic knowledge into a therapeutic product. With the current technology and state of knowledge, near-term prospects for preparing first-generation HSC-derived cRBCs with defined dosage and purity sufficient to address the needs of those difficult-to-transfuse patients with rare phenotypes or multiple alloantibodies are more than an idle hope. This relatively small “market” already relies on RBC units that are difficult to acquire and extremely expensive if available. In contrast, providing cRBCs sufficient to supplement standard RBC (or platelet) inventories will require a considerable upgrade in our scientific knowledge, culture ingredients, and equipment—and a generous additional investment in basic science and bioreactor technology. However, pluripotent hESCs have the expansion potential to provide these cell numbers and hiPSCs seem ideally suited for producing patient-specific cRBC units. Furthermore, mature, non-nucleated blood cells should elicit less medical and regulatory concern about the potential for neoplastic transformation when a cellular biologic is prepared by stimulating and expanding pluripotential cells. Such products are plausible, and if produced by the million units should even be affordable, but they are not on the near horizon.
Ex vivo production of human red cells, the Holy Gvail of blood transfusion. Professional illustration by Debra T. Dartez.
Ex vivo production of human red cells, the Holy Gvail of blood transfusion. Professional illustration by Debra T. Dartez.
Giarratana et al's findings should en-courage investigators (and funding agencies) in this field to persevere. After all, small volumes of reasonably safe and tasty beer were brewed from gravity-drained, wood-lined, copper vats even before microbes were discovered to be the source of fermentation. Scientific understanding and control of the fermentation process, coupled with stainless steel tanks and automated, microprocessor-controlled operations now provide an almost limitless source of wholesome ales and lagers of predictable flavor and body. We should aspire to no less purity and predictability in our blood supply.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal