Abstract
The best initial therapy for elderly patients with chronic lymphocytic leukemia (CLL) has not yet been defined. We investigated the activity of lenalidomide as initial therapy for elderly patients with CLL. Sixty patients with CLL 65 years of age and older received treatment with lenalidomide orally 5 mg daily for 56 days, then titrated up to 25 mg/d as tolerated. Treatment was continued until disease progression. At a median follow-up of 29 months, 53 patients (88%) are alive and 32 patients (53%) remain on therapy. Estimated 2-year progression-free survival is 60%. The overall response rate to lenalidomide therapy is 65%, including 10% complete response, 5% complete response with residual cytopenia, 7% nodular partial response, and 43% partial response. Neutropenia is the most common grade 3 or 4 treatment-related toxicity observed in 34% of treatment cycles. Major infections or neutropenic fever occurred in 13% of patients. Compared with baseline levels, we noted an increase in serum immunoglobulin levels across all classes, and a reduction in CCL3 and CCL4 plasma levels was noted in responding patients. Lenalidomide therapy was well tolerated and induced durable remissions in this population of elderly, symptomatic patients with CLL. This study was registered at www.clinicaltrials.gov as #NCT00535873.
Introduction
There is no clearly superior frontline therapy for elderly patients with chronic lymphocytic leukemia (CLL); and despite the fact that two-thirds of the patients diagnosed with CLL are older than 65 years of age,1 few studies explore the efficacy and toxicities of therapies in this population. The German CLL Study Group has conducted a trial randomizing 193 patients who were 65 years or older to receive therapy with fludarabine or chlorambucil.2 This trial demonstrated that higher response rates seen in elderly patients treated with fludarabine did not translate to improved progression-free survival (PFS) or overall survival (OS). Hillmen et al3 compared alemtuzumab and chlorambucil as initial therapy for CLL. Despite a higher overall response rate observed with alemtuzumab (76% vs 56%) in a subgroup analysis of 105 patients older than 65 years, median PFS was only 12.5 months in both treatment arms.3
Chemoimmunotherapy combinations, such as fludarabine, cyclophosphamide, and rituximab (FCR), have led to improvements in survival in younger patients with CLL and have become the standard of care in younger patients.4 When chemoimmunotherapy regimens are offered to older patients, there is often a concern for higher rates of treatment-related toxicities. According to our center's experience, patients older than 70 years treated with FCR have an increased rate of myelotoxicity and are less likely to complete 6 cycles of therapy.5 Dose-reduced purine analog chemoimmunotherapy trials, such as the “FCR-Lite” and pentostatin, cyclophosphamide, and rituximab (PCR), have been developed to reduce myelotoxicity and improve tolerability in the elderly; however, the experience is limited to a small number of patients 65 years of age or older.6,7 When therapeutic options are discussed with elderly patients, duration of response, time to disease progression, and time to next treatment may be more relevant endpoints than achieving a complete response (CR) to this group of patients.8 In addition, the impact of treatment on daily life activities and the intensity of monitoring requirements are particularly important to this population. Because of convenient oral administration and favorable toxicity profile, chlorambucil is often chosen as initial therapy for elderly patients, and reduced intensity chemoimmunotherapy combinations are being evaluated as possible alternatives.8,9
Based on the efficacy observed with lenalidomide in patients with relapsed or refractory disease,10,11 we designed this phase 2 study to explore the therapeutic potential of lenalidomide in elderly patients requiring initial treatment. Furthermore, the in vitro evidence for an immunostimulatory effect of lenalidomide on T-lymphocyte and NK-cell populations12-14 made this therapy particularly appealing for elderly patients who may experience increased morbidity with more myelosuppressive and immunosuppressive chemoimmunotherapy. The convenient oral route of administration of lenalidomide is also particularly attractive to elderly patients.
Methods
Sixty untreated patients with symptomatic CLL were enrolled in this phase 2 prospective study of lenalidomide at the University of Texas M. D. Anderson Cancer Center. All patients were age 65 years or older, had untreated CLL (58 patients) or small lymphocytic lymphoma (2 patients), and indication for treatment initiation by National Cancer Institute (NCI) Working Group criteria.15 Entry criteria also required a World Health Organization (Eastern Cooperative Oncology Group) performance of 0 to 3, and serum creatinine, bilirubin, and alanine transaminase were required to be less than or equal to twice the upper limit of normal. Patients were able to participate on this study regardless of absolute neutrophil or platelet count at the start of therapy. This study was approved by the University of Texas M. D. Anderson Cancer Center Institutional Review Board and registered at www.clinicaltrials.gov as #NCT00535873. Informed consent for participation was obtained in accordance with institutional guidelines and the Declaration of Helsinki.
Pretreatment evaluation
Pretreatment evaluation included medical history, physical examination, complete blood count with differential and chemistry profile consisting of serum creatinine, electrolytes, albumin, calcium, uric acid, lactate dehydrogenase, and alanine transaminase. Serum immunoglobulin (Ig) levels, β2-microglobulin levels, and peripheral T-cell lymphocyte subset analysis by flow cytometry were also measured. Bone marrow aspiration and biopsy were performed before therapy, including infiltration assessment, immunophenotype by flow cytometry, Ig heavy chain gene mutation analysis by polymerase chain reaction (CLL Research Consortium),16 and Zap-70 expression by flow cytometry.17 Standard metaphase karyotype analysis and genomic abnormalities were detected by fluorescent in situ hybridization (FISH) using standard CLL probes on bone marrow samples (Abbott Molecular). CCL3 and CCL4 protein levels were measured in peripheral blood plasma samples of 31 patients before therapy and at study assessment time points by quantitative enzyme-linked immunosorbent assay according to the manufacturer's instructions (R&D Systems).
Treatment schedule
Patients received lenalidomide orally at the initial dose of 5 mg daily administered continuously for 56 days (cycles 1 and 2). After day 56, the dose could be titrated up by 5 mg every 28 days to a maximum dose of 25 mg/day as tolerated. One cycle of therapy consisted of 28 days of lenalidomide. Dosing of lenalidomide could be increased to optimize response as per the treating physician's discretion and in accordance with protocol guidelines. If patients did not tolerate higher doses of lenalidomide, dosing was adjusted to the highest tolerated dose. Patients deemed at high risk for thrombotic events could receive aspirin as prophylaxis. Hematopoietic growth factor support was allowed according to American Society of Clinical Oncology guidelines.18 Allopurinol (300 mg daily) was administered as tumor lysis prophylaxis on days 1 to 14 of cycle 1. There was no mandated antibacterial or antiviral prophylaxis. Lenalidomide dose was withheld in patients experiencing Common Terminology Criteria grade 3 or 4 toxicities, and treatment was restarted at a reduced dose of lenalidomide on resolution of toxicity to grade 2 or lower.
Response and toxicity assessment
Response assessment was performed using 2008 NCI Working Group criteria after the first 3 cycles of therapy and every 6 cycles thereafter.19 Assessment included physical examination, peripheral blood examination, bone marrow aspirate and biopsy, and lymphocyte immunophenotyping on bone marrow aspirate. Computed tomography scans were not routinely performed for response assessment. Flow cytometric assessment (flow) of bone marrow aspirate using 3-color flow cytometry was performed to estimate minimal residual disease by evaluating for CD5+/CD19+ lymphocytes with light-chain restriction. Flow minimal residual disease negativity was defined as < 1% of CD5+/CD19+ coexpressing cells with normal κ-λ ratio.
Treatment was discontinued at disease progression or if patients experienced excessive toxicity. Patients who had stable disease or better after 3 cycles continued on therapy. Trial design recommended discontinuation of therapy if there was no objective evidence of response by 9 cycles of therapy, although this decision was left to treating physician's discretion. Toxicity was scored using the Common Terminology Criteria for Adverse Events Version 3.0 for toxicity and adverse event reporting (http://ctep.cancer.gov). Tumor flare was defined as painful acute lymph node enlargement or lymph node enlargement with evidence of local inflammation occurring with initiation or reinitiation of therapy. Hematologic toxicity was graded according to 2008 NCI Working Group guidelines.19
Study endpoints and statistical analysis
The primary endpoint of this study was PFS, which was defined as time from the start of therapy to death or progression of disease. Additional endpoints were OS, CR, and overall response rate (ORR), and nonhematologic toxicity. PFS and OS were calculated using Kaplan-Meier estimates, and survival estimates were compared among subgroups of patients using the log-rank test. Responses were assessed as per intention-to-treatment analysis by pretreatment characteristics and compared using Fisher exact test (2-tailed). Difference were considered significant if P was < .05. All analyses were performed on Statistica Version 6.1 (Stat-soft).
Results
Patient characteristics and response to therapy
Sixty patients were accrued between October 2007 and April 2009. Pretreatment patient characteristics are listed in Tables 1 and 2. Median age was 71 years (range, 66-85 years). The median time from diagnosis of CLL to initiation of therapy was 29 months (range, 1-202 months). The predominant indication for initiation of therapy was rapid lymphocyte doubling time for 26 patients (43%), bulky or progressive adenopathy or splenomegaly for 16 patients (27%), Rai stage III or IV CLL for 13 patients (22%), CLL related B-symptoms for 3 patients (5%), and autoimmune cytopenia for 2 patients (3%).
Patient pretreatment characteristics
| Pretreatment characteristics . | Value . |
|---|---|
| Age, y | 71 (66-85) |
| Hemoglobin, g/dL | 12.4 (8.9-16.4) |
| Platelets, ×109/L | 155 (63-464) |
| White cell count, ×109/L | 84.0 (4.9-245) |
| Lymphocytes, ×109/L | 76.4 (2.5-227) |
| Absolute neutrophils, ×109/L | 3.9 (0-22.6) |
| β2-microglobulin, mg/L | 4.3 (2-10.2) |
| Rai stage | |
| 0 | 3 (5) |
| I or II | 39 (65) |
| III | 7 (12) |
| IV | 11 (18) |
| Charlson Comorbidity Score* | |
| 0 | 6 (10) |
| 1 or 2 | 34 (57) |
| 3 or 4 | 19 (32) |
| ≥ 5 | 1 (2) |
| Sex | |
| Female | 26 (43) |
| Male | 34 (57) |
| CD38 flow | |
| < 30% | 29 (48) |
| > 30% | 30 (50) |
| Zap-70 flow (ND = 29, 48%) | |
| < 20% | 14 (24) |
| > 20% | 17 (28) |
| IGHV mutational status | |
| Mutated | 22 (37) |
| Unmutated | 33 (55) |
| FISH, bone marrow | |
| 13q deletion | 15 (25) |
| Negative | 12 (20) |
| Trisomy 12 | 13 (22) |
| 11q deletion | 14 (23) |
| 17p deletion | 6 (10) |
| Pretreatment characteristics . | Value . |
|---|---|
| Age, y | 71 (66-85) |
| Hemoglobin, g/dL | 12.4 (8.9-16.4) |
| Platelets, ×109/L | 155 (63-464) |
| White cell count, ×109/L | 84.0 (4.9-245) |
| Lymphocytes, ×109/L | 76.4 (2.5-227) |
| Absolute neutrophils, ×109/L | 3.9 (0-22.6) |
| β2-microglobulin, mg/L | 4.3 (2-10.2) |
| Rai stage | |
| 0 | 3 (5) |
| I or II | 39 (65) |
| III | 7 (12) |
| IV | 11 (18) |
| Charlson Comorbidity Score* | |
| 0 | 6 (10) |
| 1 or 2 | 34 (57) |
| 3 or 4 | 19 (32) |
| ≥ 5 | 1 (2) |
| Sex | |
| Female | 26 (43) |
| Male | 34 (57) |
| CD38 flow | |
| < 30% | 29 (48) |
| > 30% | 30 (50) |
| Zap-70 flow (ND = 29, 48%) | |
| < 20% | 14 (24) |
| > 20% | 17 (28) |
| IGHV mutational status | |
| Mutated | 22 (37) |
| Unmutated | 33 (55) |
| FISH, bone marrow | |
| 13q deletion | 15 (25) |
| Negative | 12 (20) |
| Trisomy 12 | 13 (22) |
| 11q deletion | 14 (23) |
| 17p deletion | 6 (10) |
Values are median (range) or n (%).
CD38 flow indicates CD38 expression by flow cytometry on CD19+ lymphocytes in bone marrow aspirate; Zap-70 flow, Zap-70 expression by flow cytometry on peripheral blood B-lymphocytes; IGHV, immunoglobulin variable heavy chain; and ND, not done.
Charlson et al.20
Response by pretreatment characteristics
| Patient characteristic . | N . | NCI-WG response . | |||||
|---|---|---|---|---|---|---|---|
| CR/CRi . | % . | P . | OR . | % . | P . | ||
| All | 60 | 9 | 15 | 39 | 65 | ||
| Age, y | |||||||
| 65-71 | 32 | 6 | 19 | 23 | 72 | ||
| 72+ | 28 | 3 | 11 | .48 | 16 | 57 | .28 |
| Sex | |||||||
| Female | 26 | 2 | 8 | 17 | 65 | ||
| Male | 34 | 7 | 21 | .28 | 22 | 65 | 1.0 |
| Rai stage | |||||||
| 0-II | 42 | 7 | 16 | 29 | 69 | ||
| III-IV | 18 | 2 | 12 | .71 | 10 | 56 | .38 |
| Lymph node size* | |||||||
| < 5 cm | 50 | 7 | 14 | 34 | 68 | ||
| ≥ 5 cm | 10 | 2 | 20 | .64 | 5 | 50 | .30 |
| ALC, ×109/L | |||||||
| 0-100 | 40 | 5 | 13 | 28 | 70 | ||
| > 100 | 20 | 4 | 20 | .46 | 11 | 55 | .27 |
| β2-microglobulin, mg/L | |||||||
| < 4 | 32 | 6 | 23 | 18 | 69 | ||
| ≥ 4 | 28 | 3 | 9 | .48 | 21 | 62 | .18 |
| CD38 flow, % | |||||||
| < 30 | 29 | 3 | 10 | 16 | 55 | ||
| > 30 | 30 | 6 | 20 | .47 | 22 | 73 | .18 |
| Zap-70 flow, % | |||||||
| < 20 | 14 | 1 | 7 | 8 | 57 | ||
| > 20 | 17 | 3 | 18 | .61 | 11 | 65 | .72 |
| ND | 29 | 5 | 17 | 20 | 69 | ||
| IGHV genes (ND = 5) | |||||||
| Mutated | 22 | 1 | 5 | 11 | 50 | ||
| Unmutated | 33 | 8 | 24 | .070 | 25 | 76 | .08 |
| FISH hierarchy† | |||||||
| 13q deletion | 15 | 4 | 27 | 11 | 73 | ||
| Negative | 12 | 1 | 8 | 6 | 50 | ||
| Trisomy 12 | 13 | 1 | 8 | 13 | 100 | ||
| 11q deletion | 14 | 3 | 21 | 9 | 64 | ||
| 17p deletion | 6 | 0 | 0 | .58 | 0 | 0 | .0011‡ |
| Mean dose cycles 1-6 | |||||||
| < 5 mg | 26 | 0 | 0 | 11 | 42 | ||
| ≥ 5 mg | 34 | 9 | 26 | .0038 | 28 | 82 | .0023 |
| Tumor flare | |||||||
| No | 29 | 1 | 3 | 15 | 52 | ||
| Yes | 31 | 8 | 26 | .03 | 24 | 77 | .058 |
| Patient characteristic . | N . | NCI-WG response . | |||||
|---|---|---|---|---|---|---|---|
| CR/CRi . | % . | P . | OR . | % . | P . | ||
| All | 60 | 9 | 15 | 39 | 65 | ||
| Age, y | |||||||
| 65-71 | 32 | 6 | 19 | 23 | 72 | ||
| 72+ | 28 | 3 | 11 | .48 | 16 | 57 | .28 |
| Sex | |||||||
| Female | 26 | 2 | 8 | 17 | 65 | ||
| Male | 34 | 7 | 21 | .28 | 22 | 65 | 1.0 |
| Rai stage | |||||||
| 0-II | 42 | 7 | 16 | 29 | 69 | ||
| III-IV | 18 | 2 | 12 | .71 | 10 | 56 | .38 |
| Lymph node size* | |||||||
| < 5 cm | 50 | 7 | 14 | 34 | 68 | ||
| ≥ 5 cm | 10 | 2 | 20 | .64 | 5 | 50 | .30 |
| ALC, ×109/L | |||||||
| 0-100 | 40 | 5 | 13 | 28 | 70 | ||
| > 100 | 20 | 4 | 20 | .46 | 11 | 55 | .27 |
| β2-microglobulin, mg/L | |||||||
| < 4 | 32 | 6 | 23 | 18 | 69 | ||
| ≥ 4 | 28 | 3 | 9 | .48 | 21 | 62 | .18 |
| CD38 flow, % | |||||||
| < 30 | 29 | 3 | 10 | 16 | 55 | ||
| > 30 | 30 | 6 | 20 | .47 | 22 | 73 | .18 |
| Zap-70 flow, % | |||||||
| < 20 | 14 | 1 | 7 | 8 | 57 | ||
| > 20 | 17 | 3 | 18 | .61 | 11 | 65 | .72 |
| ND | 29 | 5 | 17 | 20 | 69 | ||
| IGHV genes (ND = 5) | |||||||
| Mutated | 22 | 1 | 5 | 11 | 50 | ||
| Unmutated | 33 | 8 | 24 | .070 | 25 | 76 | .08 |
| FISH hierarchy† | |||||||
| 13q deletion | 15 | 4 | 27 | 11 | 73 | ||
| Negative | 12 | 1 | 8 | 6 | 50 | ||
| Trisomy 12 | 13 | 1 | 8 | 13 | 100 | ||
| 11q deletion | 14 | 3 | 21 | 9 | 64 | ||
| 17p deletion | 6 | 0 | 0 | .58 | 0 | 0 | .0011‡ |
| Mean dose cycles 1-6 | |||||||
| < 5 mg | 26 | 0 | 0 | 11 | 42 | ||
| ≥ 5 mg | 34 | 9 | 26 | .0038 | 28 | 82 | .0023 |
| Tumor flare | |||||||
| No | 29 | 1 | 3 | 15 | 52 | ||
| Yes | 31 | 8 | 26 | .03 | 24 | 77 | .058 |
NCI-WG indicates NCI-sponsored CLL working group criteria for response; ALC, absolute lymphocyte count; IGHV, immunoglobulin variable heavy chain; CD38 flow, CD38 expression by flow cytometry on CD19+ lymphocytes in bone marrow aspirate; Zap-70 flow, Zap-70 expression by flow cytometry on peripheral blood; and ND, not done.
Lymph node size: ≥ 5 cm by examination or computed tomography.
FISH hierarchy according to Döhner classification system listed from lowest to highest risk genomic abnormality present.
P value: 17p− versus other FISH results.
At the time of analysis, the median follow-up for all patients was 29 months (range, 1.5-38 months) and for surviving patients 31 months (range, 19-38 months). A median of 27 cycles (range, 1-41 cycles) of lenalidomide was administered. The median daily dose received by patients was 5 mg with a maximum tolerated dose of 20 mg and minimum dose of 2.5 mg. Lenalidomide daily dose was titrated up to 10 mg in 36 patients (60%) and to 15 mg or more in 8 patients (13%), although only 26 patients (43%) were able to continue on a dose of at least 10 mg for 2 or more cycles of therapy, and at last follow-up only 10 patients (17%) were still receiving 10 mg or more.
As lenalidomide was administered continuously, we analyzed responses in all patients according to best sustained response according to CLL WG 2008 criteria. By intention to treat, the ORR is 65%, including 6 patients (10%) with CR, 3 patients (5%) with CR with residual cytopenia, 4 patients (7%) with nodular PRs, and 26 patients (43%) with partial response (PR). Four patients achieved a CR with no identifiable CLL clones by bone marrow flow cytometry (negative minimal residual disease). Table 3 summarizes the ORR achieved after completion of cycles 3, 9, 15, and 21. The median time to achievement of a PR or better was 3 months (range, 3-15 months), and the median time to achievement of CR or CR with residual cytopenia was 18 months (range, 9-27 months; Table 3). Of the 54 patients who received at least 3 cycles of therapy, 19 (35%) improved their response from no objective response to PR or from PR to nodular PR or CR between cycle 3 and cycle 9; in addition, 9 of 42 (21%) and 8 of 32 (25%) patients improved their response between cycle 9 and cycle 15, and between cycle 15 and cycle 21, respectively.
NCI responses at respective assessment time points and best response achieved for all patients
| No. on Rx/ITT . | Evaluation cycle . | ||||
|---|---|---|---|---|---|
| 3 cycles, no. (%) 54/60* . | 9 cycles, no. (%) 43/60 . | 15 cycles, no. (%) 38/60 . | 21 cycles, no. (%) 35/60 . | Best response, no. (%) 60 . | |
| Response† | |||||
| CR | 0 | 1 (2) | 3 (5) | 5 (8) | 6 (10) |
| CRi | 0 | 0 | 2 (3) | 3 (5) | 3 (5) |
| nPR | 0 | 6 (10) | 4 (7) | 5 (8) | 4 (7) |
| PR | 24 (40) | 27 (45) | 27 (45) | 22 (37) | 26 (43) |
| ORR | 24 (40) | 34 (57) | 36 (60) | 35 (58) | 39 (65) |
| DC(PR) | 0 | 1 | 0 | 1 | |
| No. on Rx/ITT . | Evaluation cycle . | ||||
|---|---|---|---|---|---|
| 3 cycles, no. (%) 54/60* . | 9 cycles, no. (%) 43/60 . | 15 cycles, no. (%) 38/60 . | 21 cycles, no. (%) 35/60 . | Best response, no. (%) 60 . | |
| Response† | |||||
| CR | 0 | 1 (2) | 3 (5) | 5 (8) | 6 (10) |
| CRi | 0 | 0 | 2 (3) | 3 (5) | 3 (5) |
| nPR | 0 | 6 (10) | 4 (7) | 5 (8) | 4 (7) |
| PR | 24 (40) | 27 (45) | 27 (45) | 22 (37) | 26 (43) |
| ORR | 24 (40) | 34 (57) | 36 (60) | 35 (58) | 39 (65) |
| DC(PR) | 0 | 1 | 0 | 1 | |
Rx indicates therapy; ITT, intention-to-treat; nPR, nodular partial response; and DC(PR), discontinued in PR.
One patient not evaluable.
2008 NCI working group criteria for response.
We examined the likelihood of achieving a response according to pretreatment characteristics (Table 2). There was no statistically significant difference in CR or ORR between patients with Rai I-II or Rai III-IV disease in this study, although this analysis is limited by small numbers. Patients with 17p deletion identified by FISH (n = 6) were less likely to achieve a response compared with patients with absence of 17p deletion by FISH (P = .001; Table 2). Although patients with unmutated IGHV genes had a higher tendency to achieve a response compared with patients with mutated IGHV genes (76% vs 50%, respectively), the difference did not reach statistical significance (P = .08).
We analyzed the relationship between response rate and the average daily dose of lenalidomide tolerated within the first 6 cycles of therapy. ORR and CR rates for patients who tolerated an average dose of at least 5 mg (34 patients, ORR 82% and CR 26%) were significantly higher compared with those who received an average dose of < 5 mg (26 patients, ORR 52% and CR 3%; Table 2). As a continuous variable, higher average daily dose of lenalidomide during the first 6 cycles was associated with a higher likelihood to achieve an objective response (P < .001) or CR (P = .018). Dose-response groups are shown in supplemental Table 1 (available on the Blood Web site; see the Supplemental Materials link at the top of the online article). We compared the baseline characteristics of patients who were able to maintain higher median daily doses of lenalidomide with those who could not. Patients who could tolerate > 5 mg of lenalidomide had higher pretreatment hemoglobin level and were less likely to have 17p deletion, although the latter was not statistically significant (supplemental Table 2).
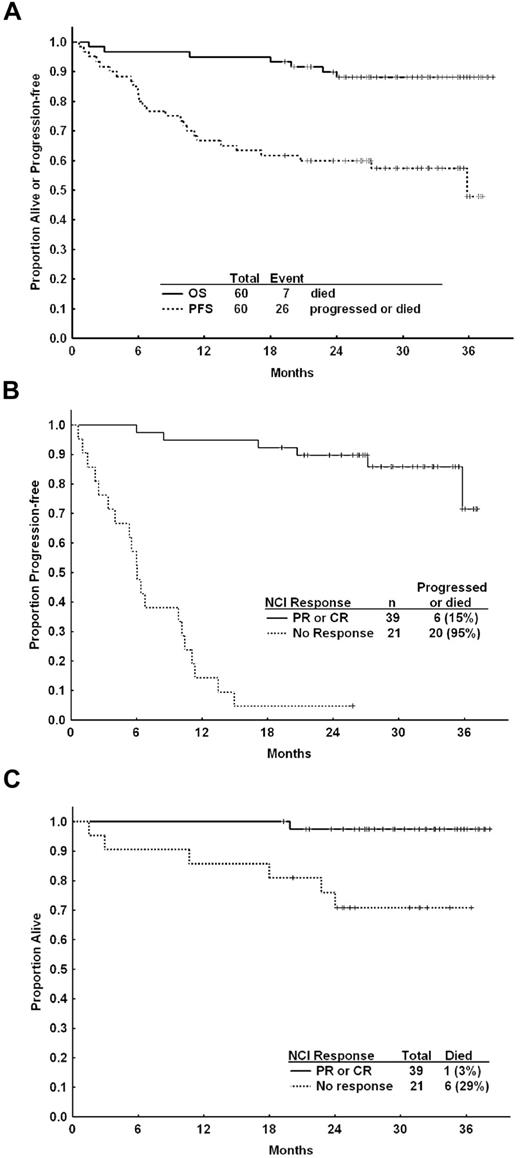
Response duration and survival
At a median follow-up of 31 months, 32 patients (53%) remain on therapy with an estimated 2-year PFS of 60% (95% CI, 46%-72%; Figure 1A). Responses to lenalidomide appeared durable with continuing therapy. Of 39 patients who achieved at least a PR, 33 patients (85%) have retained or improved their response, 5 patients (13%) have discontinued therapy in continued response because of toxicity or unrelated reasons, and 1 patient (3%) has progressed while on therapy. Eighteen patients have received subsequent therapy, including rituximab (n = 9), FCR (n = 7), and 2 patients with Richter transformation receiving oxaliplatin, fludarabine, cytarabine, and rituximab. Responses to subsequent therapy are shown in supplemental Table 3.
PFS and OS for elderly patients on lenalidomide frontline therapy. (A) PFS and OS for all patients on frontline lenalidomide therapy. At 24 months of follow-up, the median PFS was 60% and OS was 88%. (B) PFS for all patients according to achievement of PR or better compared with patients who did not achieve an objective response. (C) OS according to achievement of PR or better compared with no response.
PFS and OS for elderly patients on lenalidomide frontline therapy. (A) PFS and OS for all patients on frontline lenalidomide therapy. At 24 months of follow-up, the median PFS was 60% and OS was 88%. (B) PFS for all patients according to achievement of PR or better compared with patients who did not achieve an objective response. (C) OS according to achievement of PR or better compared with no response.
PFS was significantly shorter for the 6 patients with deletion of 17p compared with patients with other FISH results (median PFS 6 months vs not reached, P = .002). Patients who experienced a tumor flare reaction of any grade had a longer PFS than patients who did not have a tumor flare reaction (median PFS not reached vs 15 months, P = .03). The average dose of lenalidomide in the first 6 cycles of therapy was also associated with PFS. At last follow-up, only 7 of 34 patients (21%) who tolerated an average dose of 5 mg or more had progressed or died compared with 16 of 26 patients (62%) who received an average dose < 5 mg (P = .003).
Fifty-three patients (88%) are alive at a median follow-up of 31 months (Figure 1). Of the 39 patients who achieved a response, 38 (97%) are alive and 33 (85%) are progression-free. Of 7 deaths on study, 3 patients died > 18 months after starting subsequent therapy after discontinuing treatment with lenalidomide because of intolerance after < 1, 1, and 6 cycles of therapy. One patient declined further therapy after 2 cycles because of devastating social circumstances and concurrent medical issues and died 1 month later and 1 patient died after development of Richter transformation after 10 months of therapy. Two patients died of unrelated malignancies. Of the latter, one patient was diagnosed with metastatic adenocarcinoma of the colon after only 26 days of therapy who, in retrospect, had abnormal radiologic findings before study enrollment; one other patient was diagnosed with metastatic pancreatic cancer after 6 cycles of therapy; and after reviewing this patient's indications for initiation of lenalidomide, progressive anemia and 20 kg of weight loss in 6 months, the patient may have had clinical evidence of advanced malignancy before lenalidomide.
Treatment discontinuation and toxicity
Twenty-eight patients have discontinued treatment. Causes for discontinuation of therapy included lack or response or progressive disease (11 patients), lenalidomide intolerance without response (8 patients), lenalidomide intolerance or late adverse events (after 9 cycles of therapy) in patients with a response (4 patients), nonhematologic malignancy (3 patients), and patient preference (2 patients). Among patients intolerant of medication, reasons for discontinuation included rash (3 patients), shortness of breath (1 patient), fatigue (1 patient), infections (1 patient), fevers (1 patient), allergy (1 patient), or diarrhea (1 patient). Late adverse events (after 9 cycles of therapy) included a cerebrovascular accident, a veno-thromboembolic event, and pneumonia.
Therapy-associated toxicities are summarized in Tables 4 to 6. The most common toxicity was grade 3 or 4 neutropenia, which occurred in 34% of evaluable cycles. The majority of patients (83%) experienced at least one episode of grade 3 or 4 neutropenia. Grade 3 or 4 neutropenia was managed with transient interruption of therapy followed by dose reduction. Other hematologic toxicities were less common, with grade 3 or 4 thrombocytopenia and anemia occurring in only 12% and < 1% of cycles, respectively. The rate of hematologic toxicity was constant throughout treatment courses (supplemental Table 4A).
Hematologic toxicity
| Hematologic toxicity . | Grade ≥ 3, no. (%) of patients . | Grade 4, no. (%) of patients . | Grade 1 or 2, % of cycles . | Grade 3, % of cycles . | Grade 4, % of cycles . |
|---|---|---|---|---|---|
| Neutropenia | 50 (83) | 40 (67) | 38 | 24 | 10 |
| Thrombocytopenia | 28 (47) | 5 (8) | 51 | 11 | 0.7 |
| Anemia | 0 | 0 | 24 | 0 | 0 |
| Hematologic toxicity . | Grade ≥ 3, no. (%) of patients . | Grade 4, no. (%) of patients . | Grade 1 or 2, % of cycles . | Grade 3, % of cycles . | Grade 4, % of cycles . |
|---|---|---|---|---|---|
| Neutropenia | 50 (83) | 40 (67) | 38 | 24 | 10 |
| Thrombocytopenia | 28 (47) | 5 (8) | 51 | 11 | 0.7 |
| Anemia | 0 | 0 | 24 | 0 | 0 |
Eight patients (13%) experienced at least one severe (grade 3 or 4) infection or neutropenic fever, including one fatal infection (Table 5). In terms of grade 3 or 4 infections, there were 3 patients with pneumonia (4 episodes), 2 patients (3 episodes) with uncomplicated respiratory tract infections who received intravenous antibiotics because of neutropenia, and 3 patients admitted with febrile neutropenia (including 1 bacteremia episode). Four of the documented infections were associated with grade 3 or 4 neutropenia. Seven of the 9 severe infectious events occurred within the first 9 cycles of therapy (supplemental Table 4B). Minor infections were common, with 53% of patients experiencing at least one minor infection during therapy with an infection risk of 5.8% per patient course (Table 5). Minor infections included mostly upper respiratory tract infections, sinus infections, or bronchitis. The rate of minor infections was fairly constant throughout therapy (supplemental Table 4B).
Infectious toxicity
| . | Grade 1 or 2 . | Grade ≥ 3 . | ||
|---|---|---|---|---|
| No. of episodes . | No. (%) of patients . | No. of episodes . | No. (%) of patients . | |
| Infections | ||||
| Bacteremia | 0 | 0 | 1 | 1 (2) |
| Pneumonia/bronchitis | 5 | 5 (8) | 7 | 5 (8) |
| URTI | 26 | 18 (30) | 0 | 0 |
| Orodental | 3 | 2 (3) | 0 | 0 |
| Otitis/sinusitis | 8 | 8 (13) | 0 | 0 |
| UTI | 8 | 5 (8) | 1† | 1 (2)† |
| Other infections* | 6 | 5 (8) | 0 | 0 |
| Any infectious event | 56 | 32 (53) | 8 | 6 (10) |
| Neutropenic fever | 1 | 1 (2) | 3 | 3 (5) |
| Febrile, non-neutropenic | 11 | 11 (18) | 1 | 1 (2) |
| Any febrile or infectious event | 68 | 37 (62) | 12 | 8 (13) |
| . | Grade 1 or 2 . | Grade ≥ 3 . | ||
|---|---|---|---|---|
| No. of episodes . | No. (%) of patients . | No. of episodes . | No. (%) of patients . | |
| Infections | ||||
| Bacteremia | 0 | 0 | 1 | 1 (2) |
| Pneumonia/bronchitis | 5 | 5 (8) | 7 | 5 (8) |
| URTI | 26 | 18 (30) | 0 | 0 |
| Orodental | 3 | 2 (3) | 0 | 0 |
| Otitis/sinusitis | 8 | 8 (13) | 0 | 0 |
| UTI | 8 | 5 (8) | 1† | 1 (2)† |
| Other infections* | 6 | 5 (8) | 0 | 0 |
| Any infectious event | 56 | 32 (53) | 8 | 6 (10) |
| Neutropenic fever | 1 | 1 (2) | 3 | 3 (5) |
| Febrile, non-neutropenic | 11 | 11 (18) | 1 | 1 (2) |
| Any febrile or infectious event | 68 | 37 (62) | 12 | 8 (13) |
URTI indicates upper respiratory tract infection; and UTI, urinary tract infection.
Other infections: conjunctivitis (4), wound infection (1), and perirectal (1).
Infection concurrent with respiratory tract infection.
There were few grade 3 or 4 nonhematologic or noninfectious events (Table 6). Grade 1 and 2 nonhematologic or noninfectious toxicities were more common (Table 6) and included fatigue (92% of patients), diarrhea (55%), constipation (55%), rash (48%), and/or pruritus (43%). Grade 1 or 2 tumor flare reactions occurred in 31 (52%) patients, but these were generally mild and tolerated without further therapy (18 patients) or treated with short administration of nonsteroidal anti-inflammatory drugs (5 patients), steroids (9 patients), or dose adjustment of lenalidomide (10 patients). Almost all tumor flare reactions occurred within the first 3 cycles of therapy, with the majority occurring in the first cycle (supplemental Table 4C). There were no grade 3 or 4 episodes of tumor flare or any tumor lysis in this study.
Other (nonhematologic/noninfectious) toxicity
| Toxicity* . | Grade 1 or 2 . | Grade 3 or 4 . | ||
|---|---|---|---|---|
| No. of patients . | % of patients . | No. of patients . | % of patients . | |
| Fatigue | 55 | 92 | 2 | 3 |
| Diarrhea | 33 | 55 | 0 | 0 |
| Constipation | 33 | 55 | 1 | 2 |
| Tumor flare | 31 | 52 | 0 | 0 |
| Skin rash | 29 | 48 | 1 | 2 |
| Sweating | 29 | 48 | 0 | 0 |
| Pruritus | 26 | 43 | 2 | 3 |
| Cough | 24 | 40 | 0 | 0 |
| Nausea or vomiting | 23 | 38 | 0 | 0 |
| Dyspnea | 20 | 33 | 1 | 2 |
| Joint pains | 18 | 30 | 0 | 0 |
| Dizziness or syncope | 16 | 27 | 1 | 2 |
| Hyperglycemia | 18 | 30 | 1 | 2 |
| Creatinine | 15 | 25 | 0 | 0 |
| Fever, non-neutropenic | 14 | 23 | 1 | 2 |
| Dry mouth | 13 | 22 | 0 | 0 |
| Decreased appetite | 14 | 23 | 1 | 2 |
| Dry skin | 14 | 23 | 0 | 0 |
| Sensory neuropathy | 13 | 22 | 0 | 0 |
| Back pain | 13 | 22 | 0 | 0 |
| Hypomagnesemia | 12 | 20 | 0 | 0 |
| Neurologic NOS | 12 | 20 | 0 | 0 |
| Muscular pain | 12 | 20 | 0 | 0 |
| Insomnia | 12 | 20 | 0 | 0 |
| Abdominal pain NOS | 11 | 18 | 2 | 3 |
| Hyperuricemia | 10 | 17 | 0 | 0 |
| Abnormal ALT or AST | 10 | 17 | 2 | 3 |
| Hyperkalemia | 9 | 15 | 1 | 2 |
| Headache | 9 | 15 | 1 | 2 |
| Flatulence | 9 | 15 | 0 | 0 |
| Hypocalcemia | 8 | 13 | 0 | 0 |
| Heartburn | 8 | 13 | 0 | 0 |
| Skin, other lesions | 8 | 13 | 0 | 0 |
| Peripheral edema | 8 | 13 | 0 | 0 |
| Bloating/abdominal distension | 8 | 13 | 0 | 0 |
| Gastrointestinal, NOS | 7 | 12 | 1 | 2 |
| Hyperbilirubinemia | 7 | 12 | 2 | 3 |
| Weight loss | 7 | 12 | 0 | 0 |
| Muscle cramps | 6 | 10 | 0 | 0 |
| Hypokalemia | 4 | 7 | 4 | 7 |
| Toxicity* . | Grade 1 or 2 . | Grade 3 or 4 . | ||
|---|---|---|---|---|
| No. of patients . | % of patients . | No. of patients . | % of patients . | |
| Fatigue | 55 | 92 | 2 | 3 |
| Diarrhea | 33 | 55 | 0 | 0 |
| Constipation | 33 | 55 | 1 | 2 |
| Tumor flare | 31 | 52 | 0 | 0 |
| Skin rash | 29 | 48 | 1 | 2 |
| Sweating | 29 | 48 | 0 | 0 |
| Pruritus | 26 | 43 | 2 | 3 |
| Cough | 24 | 40 | 0 | 0 |
| Nausea or vomiting | 23 | 38 | 0 | 0 |
| Dyspnea | 20 | 33 | 1 | 2 |
| Joint pains | 18 | 30 | 0 | 0 |
| Dizziness or syncope | 16 | 27 | 1 | 2 |
| Hyperglycemia | 18 | 30 | 1 | 2 |
| Creatinine | 15 | 25 | 0 | 0 |
| Fever, non-neutropenic | 14 | 23 | 1 | 2 |
| Dry mouth | 13 | 22 | 0 | 0 |
| Decreased appetite | 14 | 23 | 1 | 2 |
| Dry skin | 14 | 23 | 0 | 0 |
| Sensory neuropathy | 13 | 22 | 0 | 0 |
| Back pain | 13 | 22 | 0 | 0 |
| Hypomagnesemia | 12 | 20 | 0 | 0 |
| Neurologic NOS | 12 | 20 | 0 | 0 |
| Muscular pain | 12 | 20 | 0 | 0 |
| Insomnia | 12 | 20 | 0 | 0 |
| Abdominal pain NOS | 11 | 18 | 2 | 3 |
| Hyperuricemia | 10 | 17 | 0 | 0 |
| Abnormal ALT or AST | 10 | 17 | 2 | 3 |
| Hyperkalemia | 9 | 15 | 1 | 2 |
| Headache | 9 | 15 | 1 | 2 |
| Flatulence | 9 | 15 | 0 | 0 |
| Hypocalcemia | 8 | 13 | 0 | 0 |
| Heartburn | 8 | 13 | 0 | 0 |
| Skin, other lesions | 8 | 13 | 0 | 0 |
| Peripheral edema | 8 | 13 | 0 | 0 |
| Bloating/abdominal distension | 8 | 13 | 0 | 0 |
| Gastrointestinal, NOS | 7 | 12 | 1 | 2 |
| Hyperbilirubinemia | 7 | 12 | 2 | 3 |
| Weight loss | 7 | 12 | 0 | 0 |
| Muscle cramps | 6 | 10 | 0 | 0 |
| Hypokalemia | 4 | 7 | 4 | 7 |
NOS indicates not otherwise specified; ALT, alanine transaminase; and AST, aspartate aminotransferase.
Toxicity listed if any grade 3 or 4, or grade 1 or 2 in ≥ 10% of patients.
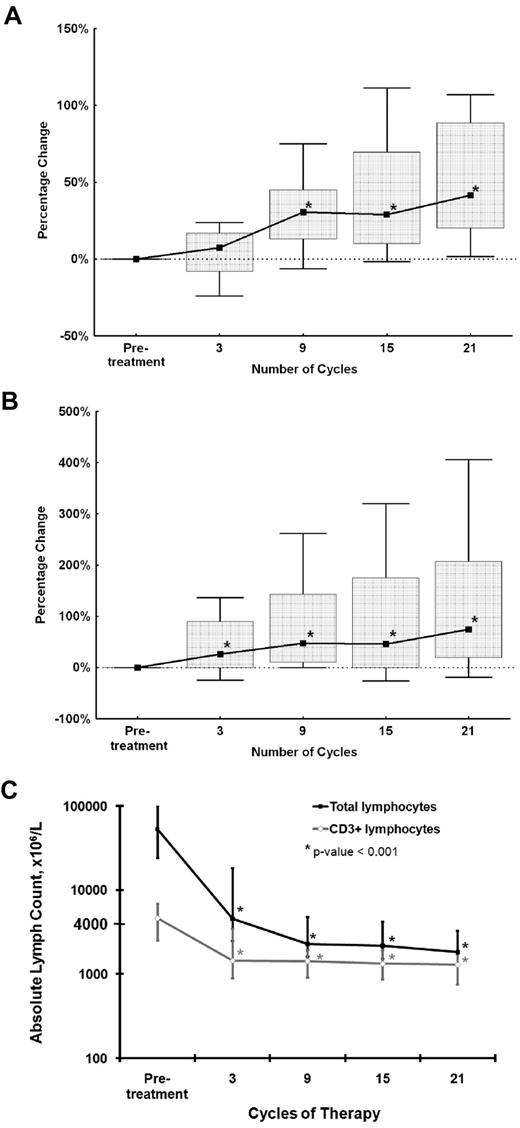
Ig levels
Serum Ig levels were measured at baseline and during treatment in the 34 patients who completed at least 15 cycles of therapy; 33 of these patients achieved an objective response. An increase in Ig levels across all Ig classes was noted (Figure 2A-B). The rise in IgG and IgA was most pronounced between 3 and 9 cycles of therapy, whereas the rise in IgM occurred by the third cycle of therapy. Sixteen patients had decreased IgG levels (< 700 mg/dL) before therapy. In 8 patients (50%), IgG levels normalized after 15 cycles of therapy, and another 3 patients (19%) demonstrated an increase in IgG of greater than 50% from baseline. As seen in Figure 2A and B, the rise in serum Ig levels was durable through therapy. We did not observe a correlation between serum Ig levels and the likelihood of developing an infectious event; however, this analysis may be limited by our small sample size.
Correlative studies of peripheral blood lymphocyte populations and serum Ig levels. *P < .001, compared with pretreatment values. (A) Serum IgG measurements as a percentage change from baseline. There is a significant increase in serum IgG from 3-9 cycles of therapy. Lines represent median percentage change in serum IgG; boxes, interquartile range; and outer spread lines, 10th to 90th percentiles. (B) Serum IgM measurements as a percentage change from baseline. There is a significant increase in serum IgM from by 3 cycles and from 3-9 cycles of therapy. Lines represent median percentage change in serum IgM; boxes, interquartile range; and outer spread lines, 10th to 90th percentiles. (C) Peripheral blood total lymphocyte and CD3+ T-lymphocyte counts for patients who completed at least 15 cycles of therapy (n = 38), including 31 patients who have completed 21 cycles. Range bars represent the interquartile range.
Correlative studies of peripheral blood lymphocyte populations and serum Ig levels. *P < .001, compared with pretreatment values. (A) Serum IgG measurements as a percentage change from baseline. There is a significant increase in serum IgG from 3-9 cycles of therapy. Lines represent median percentage change in serum IgG; boxes, interquartile range; and outer spread lines, 10th to 90th percentiles. (B) Serum IgM measurements as a percentage change from baseline. There is a significant increase in serum IgM from by 3 cycles and from 3-9 cycles of therapy. Lines represent median percentage change in serum IgM; boxes, interquartile range; and outer spread lines, 10th to 90th percentiles. (C) Peripheral blood total lymphocyte and CD3+ T-lymphocyte counts for patients who completed at least 15 cycles of therapy (n = 38), including 31 patients who have completed 21 cycles. Range bars represent the interquartile range.
Lymphocyte subset analysis
To understand the kinetics of the lymphocyte responses during lenalidomide treatment, we analyzed peripheral blood and marrow lymphocyte populations in patients who received at least 15 cycles of therapy (34 patients). All but one of these patients achieved a response to therapy. In the majority of patients, the number of total circulating lymphocytes decreased significantly during the first 3 cycles, which was sustained for the duration of therapy (Figure 2C). The absolute number of CD3+ T cells was elevated in the majority of patients before start of therapy and decreased during therapy, 27 of 34 patients (79%) attained normal absolute CD3+ T-cell counts after 15 cycles of therapy. For these patients, T-cell numbers and the proportion of CD4 to CD8 lymphocytes remained within normal limits during treatment. There was no statistically significant association between severe infections and absolute T- or B-cell numbers or subsets in the periphery or in bone marrow before therapy.
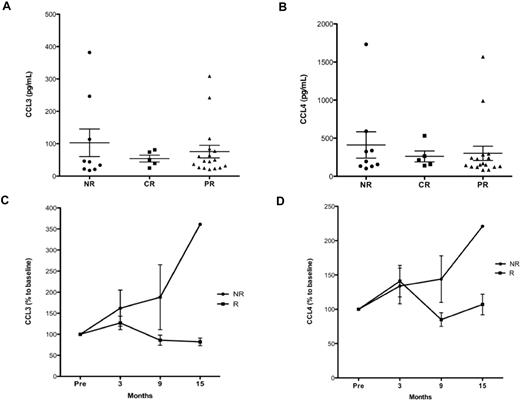
CCL3 and CCL4 analysis
CCL4 are chemokines secreted by CLL cells in the lymph node microenvironment in response to B-cell receptor (BCR) activation21,22 and can be detected in patient's plasma, where their concentrations predict for disease progression and time to first treatment.23 We analyzed CLL3 and CCL4 plasma levels in patients receiving lenalidomide to determine whether levels change during therapy. We measured plasma CCL3 and CCL4 in 31 patients before therapy and after 3, 9, and 15 cycles (n = 29, 24, and 20 patients, respectively). This included 17 patients who achieved a PR, 5 patients who achieved a CR, and 9 patients without a response. We noted no correlation between pretreatment CCL3 or CCL4 levels and likelihood of response (Figure 3A-B). Although no significant difference was observed in CCL3 and CCL4 levels after 3 cycles of therapy between responders (PR or CR) and nonresponders, after 9 cycles of therapy responders had significantly lower levels of CCL3 or CCL4 relative to pretreatment (Figure 3C-D). There were insufficient data to assess CCL3 and CCL4 levels after 15 cycles of therapy. No correlation was found between CCL3 or CCL4 levels and peripheral or bone marrow lymphocyte counts or proportion of CLL cells.
CCL3 and CCL4 serum levels before and during therapy with lenalidomide. CCL3 and CCL4 plasma levels were measured by enzyme-linked immunosorbent assay in peripheral blood samples of patients before therapy and after 3, 9, and 15 cycles of lenalidomide. (A) CCL3 levels (pg/mL) measured before therapy according to NCI response: NR, CR, and PR (mean ± SEM, 102.8 ± 42.6, 53.9 ± 10.5, and 75.6 ± 19.5, respectively) and (B) CCL4 levels (pg/mL) according to response: NR, CR, and PR (mean ± SEM, 411.5 ± 172.9, 261.4 ± 71.1, and 302.0 ± 94, respectively). There was no significant difference in CCL3 or CCL4 levels before therapy between response groups. CCL3 and CCL4 levels were also measured during therapy. (C) Although there was an increase in CCL3 levels by 3 cycles of therapy regardless of response, by 9 cycles of therapy significantly higher levels of CCL3 were noted in nonresponders compared with responders (P < .05). There were insufficient data to assess the difference between responders and nonresponders after 15 cycles of therapy. (D) Similarly, CCL4 levels increased both in responders and nonresponders after 3 cycles of therapy, but there were significantly higher CCL4 levels occurring in responders to therapy after 9 cycles of therapy with lenalidomide (P < .05). Insufficient data were available after 15 cycles of therapy for comparison. NR indicates no response (stable or progressive disease); PR, partial response; CR, complete response; and R, responders (PR or CR).
CCL3 and CCL4 serum levels before and during therapy with lenalidomide. CCL3 and CCL4 plasma levels were measured by enzyme-linked immunosorbent assay in peripheral blood samples of patients before therapy and after 3, 9, and 15 cycles of lenalidomide. (A) CCL3 levels (pg/mL) measured before therapy according to NCI response: NR, CR, and PR (mean ± SEM, 102.8 ± 42.6, 53.9 ± 10.5, and 75.6 ± 19.5, respectively) and (B) CCL4 levels (pg/mL) according to response: NR, CR, and PR (mean ± SEM, 411.5 ± 172.9, 261.4 ± 71.1, and 302.0 ± 94, respectively). There was no significant difference in CCL3 or CCL4 levels before therapy between response groups. CCL3 and CCL4 levels were also measured during therapy. (C) Although there was an increase in CCL3 levels by 3 cycles of therapy regardless of response, by 9 cycles of therapy significantly higher levels of CCL3 were noted in nonresponders compared with responders (P < .05). There were insufficient data to assess the difference between responders and nonresponders after 15 cycles of therapy. (D) Similarly, CCL4 levels increased both in responders and nonresponders after 3 cycles of therapy, but there were significantly higher CCL4 levels occurring in responders to therapy after 9 cycles of therapy with lenalidomide (P < .05). Insufficient data were available after 15 cycles of therapy for comparison. NR indicates no response (stable or progressive disease); PR, partial response; CR, complete response; and R, responders (PR or CR).
Discussion
A number of monotherapies have been explored in the frontline therapy of elderly patients with CLL. Several trials with single-agent chlorambucil have included older patients; and with some differences in doses and schedule of administration, this approach is associated with an ORR of 50%-70%, relatively few complete remissions, and an estimated PFS at 2 years of 20%-40%.2,3,24,25 Single-agent fludarabine has also been evaluated in an elderly population. In a randomized comparison of fludarabine and chlorambucil in untreated elderly patients reported by Eichhorst et al, fludarabine was not associated with significantly better PFS or OS compared with chlorambucil, despite higher overall (72% vs 51%) and CR rates (7% vs 0%).2 A study of 2-chloroadenosine in 43 elderly patients with CLL was associated with impressive response rates in 33 untreated patients (ORR 76%, CR 36%) although median PFS was relatively short (< 1 year).26 Alemtuzumab monotherapy has also been investigated in untreated patients with CLL with ORR of 70% in patients older than 65 years, but remissions were short-lasting with 2-year PFS ∼ 40%.
Single-agent bendamustine has been investigated in untreated patients with Binet B or C CLL. Response rates with this treatment were ORR 68% and CR 31% (median PFS, 21.6 months).27 The median age of the patients in the bendamustine trial, however, was 63 years, and patients older than 75 years were generally excluded. FCR has also been administered to small numbers of elderly patients; however, patients in the current study were relatively unselected, whereas patients treated with FCR were more likely to have been selected for fitness to receive therapy, making the two therapeutic approaches not easily comparable. Furthermore, the current follow-up of time of this study is significantly shorter to the one of patients treated with FCR.
Our trial is the first report of lenalidomide monotherapy for elderly patients with untreated CLL. The median age of the patients in this study is 71 years, representative of the age of presentation of CLL patients in the general community. In our study, median PFS has not been reached after 30 months of follow-up. This duration of response compares favorably with the results of studies of chlorambucil, fludarabine, or alemtuzumab monotherapy that have generally been associated with median PFS of < 2 years. The ORR rate of 65% is similar to published results for monotherapy in elderly untreated patients with CLL, and the 2-year OS rate of 88% is promising in this older patient group. This is not a comparative study; therefore, these results require confirmation with larger phase 3 trials, such as the ongoing ORIGIN trial (#NCT00910910) comparing lenalidomide with chlorambucil for previously untreated elderly patients. Furthermore, the results of phase 2 trials such as ours may vary according to patient pretreatment characteristics. The population enrolled in this trial was composed of 30% of patients with Rai stage III/IV disease, 10% with 17p deletion, and 23% with 11q deletion, not dissimilar to the patient populations in studies with chlorambucil, fludarabine, and alemtuzumab.
Overall, lenalidomide was well tolerated with neutropenia as the most common associated toxicity occurring in 34% of the cycles. Patients with neutropenia had doses withheld and/or reduced; therefore, the rate of neutropenia may have impacted on the exposure to lenalidomide and consequent efficacy. Although the rate of neutropenia was high, neutrophil recovery generally occurred spontaneously after withdrawal of therapy for 7-10 days and the overall rate of febrile neutropenic events was low. These phenomena have been well described in myeloma.28 In this setting, prophylactic G-CSF has been attempted to decrease treatment interruptions.28 Further investigation is required to examine whether addition of G-CSF may improve the overall efficacy of lenalidomide in our population.
As infections continued to be monitored throughout therapy and therapy was prolonged, the proportion of patients experiencing at least one minor infection was high despite the relatively low rate of infection per cycle. Any minor infection experienced by patients while on study (such as coryzal illnesses or uncomplicated urinary tract infections) was included in the analysis of adverse events. This may have led to a high estimation of grade 1 or 2 infections per patient not necessarily related to lenalidomide therapy. The rate of grade 3 or 4 infection was low and decreased in patients who continued therapy. Because of the small sample population, a larger study will be important to further define the rate of serious infections associated with this therapy.
Prior studies of lenalidomide have reported frequent tumor flare reactions and severe tumor lysis syndrome in patients with CLL. Patients in our study did not experience any severe tumor flare or tumor lysis on this dose regimen. Grade 1 or 2 tumor flare was common and either resolved spontaneously or responded well to simple measures, such as nonsteroidal anti-inflammatory drugs, dose reduction of lenalidomide, or corticosteroids in a minority of patients. The low incidence of severe tumor flare that we observed is probably related to the low starting dose of lenalidomide and gradual dose escalation. Interestingly, we noted that the development of tumor flare was associated with a higher likelihood of response as suggested by previously published findings in patients with CLL.29 This finding supports the recommendation to continue therapy with lenalidomide if tumor flare is not severe.
Initial therapy with lenalidomide for patients of any age with symptomatic CLL has been investigated by Chen et al.30 A total of 25 patients with a median age of 60 years were treated with an ORR of 56% and estimated 2-year PFS of 89%. This study initially explored a daily starting dose of lenalidomide of 10 mg followed by a rapid dose escalation to a targeted dose of 25 mg for 21 days of a 28-day cycle but required revisions because of the occurrence of fatal sepsis and severe tumor lysis in the initial 2 patients. The subsequent patients were treated with a lower starting dose of 2.5 mg and could reach a maximum daily dose of 10 mg. A direct comparison of our study with the results of Chen et al30 is difficult because our patients were older (median age 71 vs 60 years), received continuous versus intermittent administration of lenalidomide, and patients in our study were on treatment longer (27 vs 18 median number of cycles) and had a longer follow-up (29 vs 20.7 months). Both studies show that lenalidomide has clinical activity as initial treatment of CLL. The ORR is similar between these 2 studies (65% vs 56%), but the CR/CR with residual cytopenia rate is higher in our experience (15% vs 0%) possibly because of a higher cumulative dose administered as a result of the continuous schedule and longer duration of treatment. Finally, continuous dosing may be associated with a better tolerability profile because the intermittent schedule used by Chen et al30 resulted in rebound lymphocytosis in the rest period and recurrence of tumor flare reaction at reinitiation of therapy.
Lenalidomide exposure is associated with reversal of defective ability to form immune synapses between CLL cells and T cells31 and promotes costimulatory activation of B cells. In our study, we observed an increase in Ig levels during treatment with lenalidomide in our patients. This increased production of Igs is an interesting finding, which may be explained by enhanced B-cell costimulatory activity via activation of lymphocytes through phosphoinositide-3-kinase dependent up-regulation of CD154 as described by Lapalombella et al.32 In addition, a stimulatory effect of lenalidomide on T cells and NK cells has been demonstrated in vitro and in other hematologic malignancies.12,13,33 One study demonstrated up-regulation of costimulatory molecules, such as CD80 on CLL cells associated with T-cell activation after administration of lenalidomide in patients with CLL.34 The increase in CD80 expression correlated with tumor flare reaction, but the investigators were unable to correlate this with tumor response. NK-cell activation has also been demonstrated in lymphoproliferative disorders and myeloma.35-37 This, together with the dynamic changes noted in the repertoire of functional T cells in a subset of patients enrolled in this study,38 supports the immunomodulatory properties of this class of agents in CLL, similarly observed in other lymphoproliferative disorders after lenalidomide therapy.
Another interesting finding from our study is that responders exhibited a significant decrease in CCL3 and CCL4 levels during lenalidomide therapy compared with nonresponders. These chemokines are secreted by CLL cells after BCR signaling.21,39 Our group previously demonstrated that decreasing CCL3 and CLL4 levels are associated with response to therapy after inhibition of the BCR signaling pathway using the phosphoinositide 3′-kinase delta inhibitor CAL-10140 or the Bruton tyrosine kinase inhibitor PCI-32765.41 The increase in CCL3 and CCL4 levels in nonresponders may represent continued activation of CLL cells via BCR signaling pathways, other microenvironmental stimulating pathways, or because of an increased burden of CLL cells. These data should be confirmed by larger studies and suggest that further studies examining combinations of lenalidomide with agents targeting the BCR signaling pathways may be of interest.
In conclusion, the encouraging results with single-agent lenalidomide in this study and in preclinical data suggest that combination therapy with monoclonal antibodies should be further investigated in this setting. We have explored the efficacy of lenalidomide with rituximab as salvage therapy for CLL.42 Superior clinical activity and low toxicity have been observed when lenalidomide and rituximab were administered to patients with recurrent disease, suggesting that this may be a feasible combination to explore in the frontline setting.42 Phase 2 clinical trials are ongoing to assess the efficacy of immunomodulatory agents and rituximab in untreated patients with CLL.43-45 The role of immunomodulation in mediating the efficacy of lenalidomide remains to be investigated further in CLL patients; however, data both in vitro and in vivo suggest that this mechanism is probably important.
An Inside Blood analysis of this article appears at the front of this issue.
Presented in part at the 50th annual meeting of the American Society of Hematology, San Francisco, CA, December 6-8, 2008, and at the American Society of Clinical Oncology Annual Meeting, Chicago, IL, June 4-8, 2010.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Ms Kim Yerrow for patient care, data collection, and data management during this trial; Ms Susan Lerner for support with data collection and management; and Dr T. Kipps and the CLL Research Consortium, University of California San Diego, La Jolla, CA, for provision of data on ZAP70 and IGHV mutational status.
Authorship
Contribution: A.F. designed, performed, and analyzed the trial, provided clinical care to patients, and coauthored the paper; X.C.B. provided clinical care to patients, collected and analyzed results, performed statistical analysis, and wrote the paper; M.J.K. codesigned the trial, provided clinical care to patients, and coauthored the paper; W.G.W., S.M.O., S.F., S.M.K., and J.A.B. provided clinical care to patients, assisted in the analysis of data and development of critical themes, and coauthored the paper; S.W. performed statistical analysis and coauthored the paper; and B.-N.L., M.S., and J.R. analyzed laboratory data, performed statistical analysis, and coauthored the paper.
Conflict-of-interest disclosure: M.J.K. was a consultant for Celgene Corporation; W.G.W. was a consultant/advisory board member for Celgene Corporation; S.M.O. was a consultant for Celgene Corporation; J.A.B. was a consultant for Celgene Corporation; and A.F. received research support from Celgene Corporation. The remaining authors declare no competing financial interests.
Correspondence: Alessandra Ferrajoli, Department of Leukemia, University of Texas M. D. Anderson Cancer Center, 1515 Holcombe Blvd, Unit 428, Houston, TX 77030; e-mail: aferrajo@mdanderson.org.