Abstract
Several cell types have been suggested as giving rise to chronic lymphocytic leukemia (CLL), and these suggestions have reflected the sophistication of technology available at the time. Although there is no consensus as to the normal cellular counterpart(s) in the disease, an antigen-experienced B lymphocyte appears required based on surface membrane phenotypes and gene expression profiles. However, what is still unclear is whether a single or multiple normal precursors were stimulated to evolve into CLL and at what stage(s) this occurred. A unifying, parsimonious theory is that CLL clones with either mutated or unmutated IGHVs derive from marginal zone B cells. However, evidence for remarkably similar B-cell receptor amino acid sequence and striking differences in polyantigen and autoantigen-binding activity, found in some but not all CLL clones, challenge a single-cell derivation for CLL. In this Perspective, we summarize data regarding normal counterparts of CLL cells and suggest that a multistep process of leukemogenesis is important to consider when assigning a cellular origin for this disease. Finally, although available data do not definitively identify the cell(s) of origin, we offer possibilities for single- and multiple-cell origin models as straw men that can be improved on and hopefully lead to final answers to this puzzle.
Introduction
Over the years, several cell types have been suggested as normal counterparts for chronic lymphocytic leukemia (CLL). The complexity of these suggestions has reflected the sophistication of technology available at the time. For instance, the belief that CLL is a disease of accumulating immune incompetent cells that proliferate negligibly1 emanated from light microscopy analyses revealing cells of mostly uniform size, fitting clinical observations of a slow, inexorable increase of lymphocytes. However, with the advent of flow cytometry2 and the availability of safe, convenient ways to label dividing cells in vivo,3 these ideas were modified.4-6
Similarly, the belief that all CLL clones originate from follicular mantle B cells, based on shared surface membrane expression of CD5 and CD23, was altered when DNA sequencing analyses determined that approximately 50% of CLL clones have IGHV mutations,7,8 distinguishing these cases from follicular mantle B cells, which almost exclusively use unmutated IGVs.9,10
Technologic advances have helped refine early findings but have not provided definitive proof for the cellular origin of CLL. Recent observations suggest that the notion that CLL is a disease of one cell type needs revisiting. This Perspective aims to summarize some existing data on the cellular origin(s) of CLL, to call attention to new findings suggesting caution when assigning normal counterparts, and to propose additional possibilities about the cellular origin(s) of the disease.
Current hypotheses
Documenting that CLL clones use either mutated or unmutated IGHV genes8 and that this feature distinguishes patient subgroups with distinct clinical courses11,12 gave rise to the postulate that the 2 subgroups of CLL originated from distinct cell types with different differentiation and antigen encounter histories, consistent with a 2-cell origin model. Furthermore, several lines of evidence implicated B-cell receptor (BCR) signaling as a promoting factor that could lead to divergent cell biology and patient pathology. First, the IGHV repertoire in CLL is not random and differs between U-CLL and M-CLL as well as between CLL cells and normal B cells.7,8,13 Second, the preponderance of polyreactive and/or autoreactive BCRs, especially among U-CLL cases,14 and retention of signaling through U-CLL BCRs15,16 suggest that antigen-binding specificity and BCR signaling capacity influence clonal expansion,17-19 possibly by facilitating tumor survival and growth.
However, key microarray analyses of gene expression identified only a relatively small number of gene use differences between U-CLL and M-CLL,20,21 as opposed to thousands of differences between normal B lymphocytes and either U-CLL or M-CLL. These findings suggested a singular originating cell with additional, nongenetic promoting factors explaining differences in cellular features between U-CLL and M-CLL and their respective clinical outcomes.
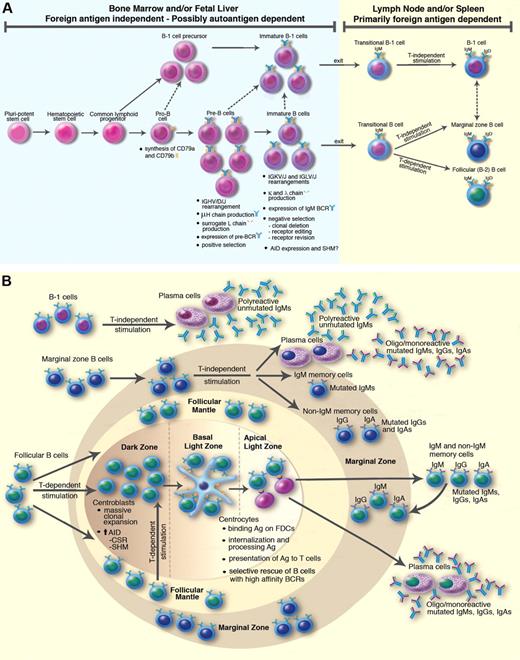
To overcome the difficulties of reconciling a 2-cell origin model, which was more consistent with BCR findings, with a one-cell model, supported by gene expression data, a unifying parsimonious theory was proposed in which both U-CLL and M-CLL derive from marginal zone (MZ) B cells.17,18 In the spleen, the MZ is an area at the outermost portion of the white pulp; MZ-like regions exist in tonsil subepithelial areas, dome regions of Peyer patches, and subcapsular regions of lymph nodes (LNs).22 MZ B cells are defined as IgMhighIgDlow cells that respond to bacterial polysaccharides in a T cell-independent manner23,24 (Figure 1). They can express either mutated or unmutated IGVs, although the proportion of cells expressing mutated genes varies depending on anatomic site, animal species, and immunization conditions.25,26 In humans, the highest proportion of IGVH mutated MZ B cells is in the spleen,27 reaching 70% to 80% (M. Colombo, F. Fais, G. Cutrona, D. Reverberi, F. Ghiotto, J. Ceccarelli, C. Tenca, S. Salvi, S. Boccardo, M. G. Calevo, A. Hadzidimitriou, K. Stamatopoulos, M. Truni, S. Bruno, M. F., manuscript in preparation). Occasionally, IGHV mutations and immunoglobulin (Ig) isotype switching occur during responses of IgMhighIgDlow B cells in MZ or MZ-like areas of humans and mice.28-31 Activation-induced cytidine deaminase (AID), the enzyme required for IGV mutations,32 could play a role in this process, although detection of AID in splenic MZ B cells is controversial.33-35 However, B cells more often do acquire such mutations, frequently along with class switch recombination, in germinal centers (GCs), and some of these B lymphocytes migrate and take up residence in MZs (Figure 1B). MZ B cells are often antigen-experienced as evidenced by clonal expansion of IgMhighIgDlow B cells without IGV mutations and by diversification and expansion in the MZ for those cells with mutations.28-31 In addition, B cells expressing IgG or IgA found in MZ and MZ-like areas36 are often referred to as switched memory B cells, use mutated IGHV, and are predominantly of post-GC origin.9,27,37
Maturation of B lymphocytes. This schema is compiled from information derived from murine and human studies of B-cell differentiation. Note that the B-1 cell lineage has not been identified in humans; therefore, the scheme is based on information from mouse studies. The schema is not all-inclusive; it focuses on issues relevant to the discussion of possible precursors of CLL cells. (A) Normal B-lymphocyte maturation occurs in 2 phases: “foreign antigen independent,” occurring primarily in fetal liver or bone marrow (depending on species); and “primarily foreign antigen dependent,” occurring in the periphery in LNs and spleen. Autoantigen interaction could influence B cells expressing complementary BCRs during both phases in positive and negative manners, although the extent to which this occurs remains unresolved. For classic (non–B-1 cell) B-lymphocyte maturation, BCR-mediated signaling is important from at least the pre–B-cell stage of differentiation when a BCR composed of a rearranged and translated IGHV/D/J rearrangement associates with the monomorphic surrogate L chain. BCR-mediated signaling through this receptor is either constitutive or induced by binding of autologous epitopes within the local environment; in the latter case, the diversity of the bound epitopes is limited because not all translated IGHV/D/J rearrangements associate with the translated surrogate L-chain receptor and also because the monomorphic structure of translated surrogate L chain does not provide antigen-binding diversity. Engagement of this receptor leads to positive selection and clonal amplification of B-cell precursors with restricted IGHV/D/J structures that can be autoreactive. At the immature B-cell stage of maturation, when translated IGHV/D/J and IGK/J or IGL/J rearrangements are paired, negative selection for higher-affinity autoreactive BCRs occurs; this process involves clonal deletion, receptor editing of the rearranged κ or λ L chain, or receptor revision of the IGHV gene. It is assumed that the same process occurs for cells of the B-1 lineage. Note that some B lymphocytes with low affinity for autoantigens do exit to the periphery. Thus, in the normal setting, B cells with no or low affinity for autoantigen move to the periphery as transitional B cells. These cells are selected into the mature B-cell repertoire as either MZ B cells or follicular (FO) B cells by T cell-independent or T cell-dependent BCR stimulation, respectively. At this step, smIgD appears. It is assumed that T cell-independent signaling is important for B-1 cells in this regard. (B) Illustration of GC and some of the consequences of antigen experience of B-1 cells, MZ B cells, and FO B cells. MZ B cells (IgMhighIgDlow) take up residence in the MZ of the spleen or MZ-like areas in human tonsillar subepithelial areas, dome regions of Peyer patches, and subcapsular regions of LNs. When they encounter T cell-independent antigens, they can respond without undergoing isotype class switching or IGV gene mutations and give rise to plasma cells secreting polyreactive, unmutated IgMs that serve as protectors from virulent microbes or eliminators of catabolic autologous molecules. MZ B cells can undergo isotype class switching or IGV gene mutation, again giving rise to plasma cells that produce oligoreactive/monoreactive Igs. Switched and nonswitched memory cells can be generated as well. B-1 cells, like MZ B cells, respond to T-independent stimulation and give rise to plasma cells producing primarily polyreactive unmutated IgMs that provide protection against infections and remove cellular debris. See the text for suggestions that B-1 cells and MZ cells, when antigen experienced, could be “memory-like.” FO B cells are the main source of mutated, isotype switch protective Igs. When these cells bind foreign antigen within (follicular mantle) or outside (blood or lymph) solid tissues, they migrate to LNs or spleen and, with the help of nonlymphoid cells and T cells, build GCs and initiate GC reactions. Within the dark zone, activated FO cells (centroblasts) down-regulate BCRs and expand at an extremely rapid rate, acquiring IGV mutations with each round of cell division. Subsequently, cells move into the basal light zone where they re-express BCRs (centrocytes) and have the opportunity to bind the initial stimulatory foreign antigen that is held in its native state on the surface of follicular dendritic cells. Those cells with BCRs that can bind these antigens are provided with a temporary survival signal; access to these antigens is limited and in this way B cells with higher affinity for the antigen are preferentially selected to avoid apoptosis and proceed to the apical light zone. In this area, B cells that have bound the initiating antigen express fragments on their cell surfaces, associated with major histocompatibility complex class II molecules, and receive a permanent survival signal from antigen-specific T cells (“follicular T cells”). The affinity-matured, often isotype-switched B cells then differentiate into plasma cells and produce oligoreactive/monoreactive Igs or become memory cells; some of these memory cells migrate to the MZ and to the bone marrow (latter not shown). Finally, AID, the enzyme required for IGV mutations and isotype class switching, is definitely expressed in FO B cells during GC reactions. It is still unclear whether AID is expressed in human B cells at more immature stages of maturation (eg, immature B cells and transitional B cells; A) or that mature down different pathways (eg, MZ B cells and B-1 cells; B).
Maturation of B lymphocytes. This schema is compiled from information derived from murine and human studies of B-cell differentiation. Note that the B-1 cell lineage has not been identified in humans; therefore, the scheme is based on information from mouse studies. The schema is not all-inclusive; it focuses on issues relevant to the discussion of possible precursors of CLL cells. (A) Normal B-lymphocyte maturation occurs in 2 phases: “foreign antigen independent,” occurring primarily in fetal liver or bone marrow (depending on species); and “primarily foreign antigen dependent,” occurring in the periphery in LNs and spleen. Autoantigen interaction could influence B cells expressing complementary BCRs during both phases in positive and negative manners, although the extent to which this occurs remains unresolved. For classic (non–B-1 cell) B-lymphocyte maturation, BCR-mediated signaling is important from at least the pre–B-cell stage of differentiation when a BCR composed of a rearranged and translated IGHV/D/J rearrangement associates with the monomorphic surrogate L chain. BCR-mediated signaling through this receptor is either constitutive or induced by binding of autologous epitopes within the local environment; in the latter case, the diversity of the bound epitopes is limited because not all translated IGHV/D/J rearrangements associate with the translated surrogate L-chain receptor and also because the monomorphic structure of translated surrogate L chain does not provide antigen-binding diversity. Engagement of this receptor leads to positive selection and clonal amplification of B-cell precursors with restricted IGHV/D/J structures that can be autoreactive. At the immature B-cell stage of maturation, when translated IGHV/D/J and IGK/J or IGL/J rearrangements are paired, negative selection for higher-affinity autoreactive BCRs occurs; this process involves clonal deletion, receptor editing of the rearranged κ or λ L chain, or receptor revision of the IGHV gene. It is assumed that the same process occurs for cells of the B-1 lineage. Note that some B lymphocytes with low affinity for autoantigens do exit to the periphery. Thus, in the normal setting, B cells with no or low affinity for autoantigen move to the periphery as transitional B cells. These cells are selected into the mature B-cell repertoire as either MZ B cells or follicular (FO) B cells by T cell-independent or T cell-dependent BCR stimulation, respectively. At this step, smIgD appears. It is assumed that T cell-independent signaling is important for B-1 cells in this regard. (B) Illustration of GC and some of the consequences of antigen experience of B-1 cells, MZ B cells, and FO B cells. MZ B cells (IgMhighIgDlow) take up residence in the MZ of the spleen or MZ-like areas in human tonsillar subepithelial areas, dome regions of Peyer patches, and subcapsular regions of LNs. When they encounter T cell-independent antigens, they can respond without undergoing isotype class switching or IGV gene mutations and give rise to plasma cells secreting polyreactive, unmutated IgMs that serve as protectors from virulent microbes or eliminators of catabolic autologous molecules. MZ B cells can undergo isotype class switching or IGV gene mutation, again giving rise to plasma cells that produce oligoreactive/monoreactive Igs. Switched and nonswitched memory cells can be generated as well. B-1 cells, like MZ B cells, respond to T-independent stimulation and give rise to plasma cells producing primarily polyreactive unmutated IgMs that provide protection against infections and remove cellular debris. See the text for suggestions that B-1 cells and MZ cells, when antigen experienced, could be “memory-like.” FO B cells are the main source of mutated, isotype switch protective Igs. When these cells bind foreign antigen within (follicular mantle) or outside (blood or lymph) solid tissues, they migrate to LNs or spleen and, with the help of nonlymphoid cells and T cells, build GCs and initiate GC reactions. Within the dark zone, activated FO cells (centroblasts) down-regulate BCRs and expand at an extremely rapid rate, acquiring IGV mutations with each round of cell division. Subsequently, cells move into the basal light zone where they re-express BCRs (centrocytes) and have the opportunity to bind the initial stimulatory foreign antigen that is held in its native state on the surface of follicular dendritic cells. Those cells with BCRs that can bind these antigens are provided with a temporary survival signal; access to these antigens is limited and in this way B cells with higher affinity for the antigen are preferentially selected to avoid apoptosis and proceed to the apical light zone. In this area, B cells that have bound the initiating antigen express fragments on their cell surfaces, associated with major histocompatibility complex class II molecules, and receive a permanent survival signal from antigen-specific T cells (“follicular T cells”). The affinity-matured, often isotype-switched B cells then differentiate into plasma cells and produce oligoreactive/monoreactive Igs or become memory cells; some of these memory cells migrate to the MZ and to the bone marrow (latter not shown). Finally, AID, the enzyme required for IGV mutations and isotype class switching, is definitely expressed in FO B cells during GC reactions. It is still unclear whether AID is expressed in human B cells at more immature stages of maturation (eg, immature B cells and transitional B cells; A) or that mature down different pathways (eg, MZ B cells and B-1 cells; B).
Interestingly, IgMhighIgDlowCD27+B cells sharing a phenotype of MZ B cells exist in the blood of normal people. Because these cells are lacking in splenectomized and congenitally asplenic persons, they may be of splenic MZ origin.23,24,38 Additional evidence supporting an MZ cell origin for IgMhighIgDlowCD27+ B cells is their presence in patients with crippling mutations of the CD40L gene, whose lymphoid tissues are virtually depleted of GCs.39,40 Interestingly, these B cells were detected in an AID-deficient patient, although they lacked IGHV mutations.37
However, an MZ origin for CLL cells faces difficulties. For example, although MZ B cells express surface IgM and IgD, as most CLL clones do, they are CD5−CD23−CD22+,23 a surface phenotype differing from CLL cells. This phenotypic difference could reflect up-regulation of CD5 and CD23 that occurs on activation.41-43 The issue of cell activation is relevant because comparisons of surface phenotypes of neoplastic and normal B-cell subsets are often used to trace normal counterparts in lymphoproliferative disorders. CLL cells are constitutively activated, as assessed by surface activation marker analyses4 and gene expression profiles,20,21 making phenotypic comparisons risky as substantial changes occur with stimulation. In addition, U-CLL cells differ from M-CLL cells in their extent and apparent timing since activation.4
Differential expression of activation markers has been useful as clinical predictors of outcome. For example, ZAP-70 and CD38 are expressed by normal B cells at specific stages and are more frequently detected on U-CLL than M-CLL cells.44-47 Similar considerations apply to predictors less frequently used in clinical settings, such as CD49d, LPL, CD69, telomerase, and receptors for several cytokines.48 However, these markers are not helpful in tracing normal counterparts of CLL cells.
New findings to be reconciled with single- and multiple-cell models of CLL derivation
Since the proposal of an MZ origin for CLL cells, several findings have emerged that require consideration.
Many U-CLLs and some M-CLLs produce natural antibodies
The antigen specificities of CLL BCRs are often skewed toward polyreactivity, which permits binding to autoantigens as well as exoantigens.14,49-53 These antigen-binding features are akin to “natural antibody” activity of the primary B-cell repertoire.54 Indeed, it has been postulated that developing B cells are inherently autoreactive,55 a feature lost on antigen-driven clonal selection and somatic IGV mutations that occur during GC reactions.56 This could explain the greater level of polyreactivity and autoreactivity of U-CLL and why antibodies produced from M-CLL rearrangements can display polyreactivity after their IGHVs are reverted to the germline sequence.14,57
Furthermore, some CLL BCRs/Igs react with antigenic targets on apoptotic cells or on proteins and lipoproteins modified by catabolic reactions.52,53,58,59 These same Igs may also bind microbes, and this is in some instances inhibited by modified protein and lipoprotein antigens.52,53
Collectively, these data are consistent with the idea that at least those cases exhibiting polyreactivity/autoreactivity derive from B lymphocytes producing natural or polyreactive antibodies. Although IGV mutations can lead to polyreactive B cells,57,60 this property is more often a function of the germline B-cell repertoire.
Stereotyped BCRs exist in approximately 30% of CLL cases, primarily U-CLL
Some CLL clones share BCRs of remarkably similar amino acid sequence.61-67 These “stereotyped” BCRs exhibit highly homologous HCDR3s, often coded by identical IGHV, IGHD, and IGHJ segments. Furthermore, many stereotyped BCRs use the same IGKV or IGLV, such that the KCDR3s and LCDR3s are also very similar in protein structure. Indeed, selection for similarity in amino acid sequence can be found even in CLL clones that do not use the same IGVs.62 The likelihood that these rearrangements are shared in different CLL B cells by chance is extremely remote (< 1 × 10−6 to < 1 × 10−12). Such stereotyped BCRs can be found on murine B-1 cells68,69 and in murine mAbs reactive with defined chemical (haptenic) antigens.70 Because only approximately 30% of CLL cases express stereotyped BCRs,67 CLL clones appear to be of 2 types, with or without stereotyped BCRs,71 suggesting at least a 2-cell derivation of CLL clones.
Most BCRs exhibiting stereotypy are in U-CLL cases; nevertheless, polyreactivity is not restricted to stereotyped antigen-binding sites. Indeed, stereotypy may indicate a level of selectivity for certain antigenic structures, exemplified by those BCRs that react with a subset of apoptotic cells expressing myosin heavy chain IIA.59 Thus, stereotyped CLL cases could derive from a set of B lymphocytes evolutionarily selected and somatically expanded for an ability to clear catabolic material and to enable the host to respond to antigens on potentially lethal bacteria and viruses,72-75 features ascribed to the murine B-176 and MZ77 compartments.
B-1 cells are self-renewing CD5+ B cells abundant in the peritoneal cavities of mice that produce polyreactive or natural antibodies.76 Although these cells respond to T-independent antigens, they rarely accumulate IGV mutations or switch to production of non-IgM isotypes, although switching can occur.78 The strength of BCR-mediated signals needed to activate B-1 cells differs from MZ B cells and follicular B cells (B1 > FO > MZ)25 and B-1 cells, like MZ B cells, are positively selected based on BCR (auto)antigen binding.79-81 B-1 cells are considered a first line of humoral defense against microbes and are distinct from follicular (B-2) cells that mount high affinity, isotype switched responses to incoming pathogens.77 It remains unclear whether there is a distinct B-1 lineage with unique genetic programs76 or whether such cells are induced by BCR-antigen interactions,82 although a precursor for murine B-1 cells has been reported.83
To date, human B lymphocytes with the features of murine B-1 cells have not been isolated; these characteristics include expression of CD5, production and spontaneous secretion of polyreactive antibodies coded by unmutated, often stereotyped IGHV/D/J rearrangements, and lacking T-cell dependence for B-cell maturation. Although human CD5+ B cells exist84,85 in the circulation, in the mantles of lymphoid follicles, and possibly in the omentum,86 the majority of these cells do not exhibit features expected of B-1 cells. IgM antibodies produced by CD5+ cells in adult human blood are usually not polyreactive, although coded by unmutated IGHVs.14,87 Furthermore, human CD5+ B lymphocytes do not proliferate or mature into plasma cells when stimulated by T-cell type II independent antigens.10 Finally, stereotypy is not found when CD5+ (and CD5−) B lymphocytes from normal adults are analyzed by DNA sequencing,88 although recently normal blood B cells expressing mRNA transcripts coding stereotyped rearrangements were identified.89
CLL cells as antigen-experienced, “memory-like” B lymphocytes
Enrichment for relatively unique antigen-binding sites and antigen-binding features suggests that CLL cells are antigen-experienced,4 resembling memory B cells.20 The classic definition of immunologic memory posits that B lymphocytes, previously exposed to foreign antigen, respond more rapidly to a second antigenic challenge with antibodies that provide a more specific and effective program for self-preservation. This definition assumes the expansion of B cells producing antibodies with more avid antigen-binding sites (created by IGV mutations) associated with switched (non-IgM) isotypes having a greater array of effector functions and diffusing more readily into tissues. This meaning clearly fits T cell-dependent, adaptive immune responses in which classic GC reactions occur, leading to lasting genetic IGV changes.
However, this definition may be too rigid for immune responses that are more innate, such as those triggered by polyreactive autoantigens or elicited by lipopolysaccharide (type I) or polysaccharide (type II) T cell-independent antigens.77 These responses generate an enhanced number of cells recognizing the stimulating antigen without necessarily inducing mutations in IGV genes; and when mutations do occur,29,90 they do not necessarily lead to increased affinity for these antigens.91 On rechallenge with the same antigen, the response might be more effective because increased numbers of cells respond, perhaps more rapidly because of epigenetic changes in the clones. However, these responding cells do not have all the characteristics required by the “memory B cell” definition, including production of increased affinity, isotype switched antibodies, although a type II T-independent memory B-cell response has been documented in mice.92
Furthermore, the definition of “antigen-experience” need not be restricted to mature B lymphocytes reacting with foreign antigen and might apply to any cell, regardless of maturation stage, that expresses a BCR or a pseudo-BCR (μH chain plus surrogate L chain) with (auto)antigen-binding potential, as long as an intact signaling system exists and survival signals are available. This notion is consistent with positive and negative selection occurring during normal B-cell development93 (Figure 1A).
Therefore, there may be several kinds of “antigen-experienced” B cells, only some of which fulfill the classic memory B-cell definition. In this regard, M-CLL cells could be similar to “classic memory B cells,” generated either by a typical GC-based reaction or by a response outside GCs that induces IGV mutations.29,36,90 In contrast, U-CLL cells could be viewed as antigen experienced, “memory-like” cells that at one of several stages in B-cell maturation could not or failed to change their antigen combining sites despite repeated stimulation.
Certain miRNA loci are deleted or inactivated in CLL
Micro-RNAs (miRNAs) are small, noncoding RNAs that inhibit protein synthesis, either directly by altering mRNA transcription or indirectly by causing mRNA degradation.94 A detailed discussion of miRNA features and functions goes beyond the scope of this Perspective, and the reader is referred to recent excellent reviews.94-97 However, a few points deserve comment.
First, the targets of miRNAs are often genes involved in cell cycle regulation, apoptosis, or angiogenesis; therefore, miRNAs can function as either tumor suppressor genes or as oncogenes, depending on their level of expression or functional abilities. Second, because mutation/inactivation of a single miRNA is recessive, the effect of mutation of one miRNA allele is most obvious in cells with loss or dysfunction of the other allele, in line with the classic Knudson definition of tumor suppressor genes.
The relevance of miRNA to CLL originated with finding that 2 miRNAs (miR15a and miR16-1) were frequently lost in the 13q deletion found in more than 60% of CLL cases98 and that a germline mutation affecting the miR15/16 gene cluster occurred in patients with familial CLL.99 Moreover, New Zealand Black mice, which spontaneously develop a lymphoproliferative disorder resembling human CLL based on leukemic cell phenotype, have the same germline miRNA defect.100 Similarly, mice with a deletion of the DLEU2/miR-15a/16-1 cluster develop a disease closely resembling human CLL.101
Notably, each of the common chromosomal abnormalities in human CLL potentially leads to changes in regulatory functions of miRNAs. For example, miR34b and miR34c can be lost with an 11q deletion102,103 and miR34a with a 17p deletion.95,104 Furthermore, monoallelic98 or biallelic103,105,106 deletion/inactivation of miR15/16 leads to high Bcl-2 expression in CLL and to enhanced cell growth and cell cycle progression. In addition, miR29a/29b and miR181a/181b are involved in modulating expression of TCL1,107 which activates AKT and influences pathways involved in apoptosis and proliferation. These deletions are not infrequent in CLL and transgenic mice overexpressing TCL1 in B cells develop a lymphoproliferative disorder resembling U-CLL.108,109 Thus, the miR-15a/16-1 cluster, miR29a/29b, and miR181a/181b appear to function as tumor suppressor genes, and their inactivation could up-regulate genes involved in leukemogenesis.
In contrast, some miRNAs can be up-regulated in CLL cells, for example, miR-21 and miR-181a,95 potentially leading to modulation of other genetic pathways. In these less frequent instances, miRNAs have an oncogenic rather than an antioncogenic function.
Epigenetic modifications in CLL
Epigenetic alterations in cell genomes can contribute to a malignant phenotype, and these changes can be transmitted from parental to daughter cells, “somatic transmission.” Of interest, these changes can also occur in germline cells and be transmitted from one generation to another,110 consequently influencing CLL risk.111 Because large family pedigrees with CLLs are rare,112 few data exist about acquired changes passing through generations. A recent report indicated that alterations within chromosome 14q1 associated with familial, but not sporadic, CLL.113 Furthermore, in a study of a large, CLL-affected family, Death-associated protein kinase 1 (DAPK1), which is often methylated in both sporadic and familial CLL, was a predisposing gene. Affected members of this family showed a single nucleotide polymorphism within the promoter region of DAPK1 that silenced this gene by binding the transcriptional regulator HOXB7.114 This heritable mutation might explain methylated DAPK1 in familial CLL and suggests a contribution of trans-generational epigenetic events in the development of CLL.
Epigenetic profiles of CLL clones have been analyzed more extensively in sporadic CLLs, where somatic alterations are common. These epigenetic changes, including global DNA hypomethylation that could cause genomic instability, and CpG island hypermethylation that could alter gene expression, may be important in CLL.115 Furthermore, aberrant DNA methylation exists at the preleukemic stage in TCL-1 CLL-like leukemias, and methylated genes accumulate as disease progresses to the leukemic stage.116
Because DNA methylation is heritable, the comparison in global DNA methylation profiles generated from M-CLL and U-CLL patient samples might provide a hint as to one-cell versus 2-cell models of CLL derivation. Although no association between IGHV mutation status and DNA methylation of CpG islands was found in 2 instances,117,118 a genome-wide methylation array analysis on M-CLL and U-CLL samples119 suggested distinct DNA methylation patterns in a small subset of genes between the 2.
First-degree relatives of CLL patients have a higher likelihood of developing oligoclonal/monoclonal B cells than nonrelatives
Oligoclonal/monoclonal expansions of B lymphocytes (monoclonal B-cell lymphocytosis [MBL]), some with a typical CLL surface phenotype, can be found in the blood of approximately 13% of relatives of CLL patients.120 MBLs occur at a lower frequency (∼ 3%) in apparently healthy persons without a family history of CLL.121,122 Chromosomal abnormalities seen in CLL can be found in these expansions.123 In familial CLL, family members with MBL or CLL may manifest a clone with different BCR structure and IGHV mutation status from that of other family members,124,125 suggesting divergence between genetic changes determining a cell's leukemic status and promoting factors determining a cell's level of expansion, which can be influenced by BCR specificity. Because some MBLs do not express surface CD5,122 they more closely resemble precursors of other non-Hodgkin lymphomas (NHLs).
Collectively, these findings suggest an inherited susceptibility to developing clones of B lymphocytes in CLL family members, which exceeds the numeric boundaries of most healthy subjects, and this susceptibility can lead to different types of expansions depending on other factors that are not clear at this juncture (eg, subset of B cells driven to expand, classes of antigens driving the expansion). This susceptibility could be the result of inherited differences in the primary structure of alleles controlling key functions in B lymphocytes or the result of epigenetic changes, passed from one generation to another, that alter such alleles. In addition, because these oligoclonal/monoclonal expansions can lead to CLL and possibly other NHLs over time in a small number of patients (∼ 1%/year),123 it is plausible that CLL requires several genetic abnormalities before complete leukemic transformation. This process and timing are reminiscent of that exemplified by other NHLs.126
For example, in Burkitt lymphoma and follicular lymphoma, the initial transformation event may occur at the pro–/pre–B-cell level because cells share identical myc (t8;14) or bcl-2 (t14;18) rearrangements with genes of the Ig locus.127 However, within BL and follicular lymphoma clones, subclones exhibit unique point mutations within the clonal IGHV/D/J rearrangement.128-130 Because ongoing point mutations occur most frequently in GCs, both lymphomas could emanate from GC cells, a hypothesis supported by the centroblast (Burkitt lymphoma) and centrocyte (follicular lymphoma) phenotypes of the respective cells. Furthermore, because recombination events, such as isotype switching and perhaps receptor editing and revision occur in GCs, those lymphomas with rearrangements between myc or bcl-2 and switch regions could arise in a mature GC cell.131,132 Furthermore, more than 50% of normal persons have 0.1-10/106 lymphocytes exhibiting t(14;18),126 and most of these involve switch regions, suggesting they occurred in GCs, possibly in cells undergoing class switch recombination on the other allele. Finally, it is noteworthy that, even though half the population carry B cells with t(14;18), only approximately 1 of 24 000 people develops full-blown follicular lymphoma.133
Thus, transformation in some lymphomas can span a long period, does not reach completion in all persons, and likely requires additional signals, such as antigenic stimulation via an intact BCR signaling pathway and exposure to a variety of cytokines to do so. In addition, transforming events can occur at different stages of B-cell maturation (eg, from pro-/pre-B cells to GC B cells). In such circumstances, which cell should be indicated as the cell of origin: the GC cell, where full-blown transformation may have occurred, or the early B cell, where one of the most important lesions may have taken place? Furthermore, must the intervening genetic abnormalities occur at defined, discrete stages of B-cell maturation (as does the final transforming event) or can these abnormalities be acquired randomly, depending on the type or efficiency of promoting events causing them?
These same considerations relate to CLL. Indeed, longitudinal studies suggest that 13q deletions often appear earlier in the disease than other alterations115,134 and, as mentioned, this deletion is seen in some persons with MBL, which can be a preleukemic state.123 Thus, leukemogenesis in CLL may also follow a stepwise pattern like other lymphomas, whereby each step leads to acquisition of increasingly malignant properties.
How might one reconcile dilemmas raised by new data?
The following new observations need to be melded with data that led to the current hypotheses regarding the cell(s) of origin in CLL: (1) “preleukemic” MBLs occur at a considerably higher rate in CLL relatives; (2) antigen-binding characteristics of CLL BCRs differ considerably between U-CLL and M-CLL; (3) stereotyped BCRs, suggesting an evolutionary difference in B-cell subsets, are found in certain CLL clones but not in others; (4) abnormalities of several miRNAs exist in many CLLs, and these can be somatic or germline-encoded; (5) methylation changes can be transferred vertically in families; and (6) other NHLs can develop in a stepwise manner over time.
Focusing on the last point and trying to include the previous points, a sequential process of CLL leukemogenesis can be envisioned. If the genesis of CLL is like other B-cell lymphomas, then this process will require a series of transforming events, occurring over time, during which preleukemic cells survive or are kept alive by signals delivered by the microenvironment. The transforming events in CLL might involve structural changes in regulatory genes or epigenetic regulation of structural genes. Hence, leukemogenesis could be a long process spanning several steps in B-lymphocyte development (Figure 1).
The evolving transforming events would be pressed forward by microenvironmental factors that promote acquisition of additional lesions. These promoting activities, occurring primarily in proliferation centers of peripheral lymphoid organs and bone marrow, could facilitate growth or block death by providing essential cell-cell and cell-soluble factor interactions. For some CLLs, a promoting factor could be engagement of structurally constrained BCRs by antigens of appropriate affinity that support survival and/or expansion.17,18 Recent repertoire studies demonstrate an imbalance of IGV genes not only in CLLs but also in splenic MZ lymphoma135 and particularly in mantle cell lymphomas136 for which evidence exists that the major transforming translocation may occur among pro-/pre-B cells137 (Figure 1A). Thus, antigenic selection may operate for several lymphoproliferative disorders, in which BCR engagement by restricted, albeit probably different, antigenic epitopes promotes survival and growth of developing malignant clones. However, promoting events would not be limited to antigenic stimulation because evolving leukemic clones, as seminormal B lymphocytes, could be influenced by all of the other receptor and cytokine/chemokine interactions to which a normal B cell would respond.
The following scenario adds details to this general scheme. An early lesion occurs in a B lymphocyte that favors growth or survival. The stage of B-cell maturation at which this initial abnormality occurs could vary. For familial CLL, this would probably be an inherited trait present in the germline or a transmitted epigenetic modification that changes a normal function of specific genes. For sporadic CLL, somatic lesions could occur at virtually any point in B-cell development (Figure 1). This difference in the point at which the abnormality occurs is consistent with the approximately 4-fold higher likelihood of developing MBL in relatives of CLL patients,120 as such persons would start life with this propensity, as opposed to acquiring it in sporadic CLL.
Even with appropriate promoting factors, this initial event would not lead to overt CLL, consistent with only a minor subset of MBL patients developing CLL and at a very slow rate. Other abnormalities would need to arise over time in a B cell with such an initial genetic aberration. For example, development of a defect in tolerance induction, such as the inability to delete autoreactive BCRs, might lead to selection of unique antigen-binding sites, common in approximately 30% of patients. Instead, inappropriate provision of T lymphocyte or accessory cell “help” to autoreactive cells in the normal B-cell repertoire could lead to the same result. Both would provide an effective, autoantigenic drive to B cells with structurally constrained BCRs, some of which could have undergone various types of receptor reconfiguration and yet retained inappropriate antigen-binding properties.138 An alternative, not mutually exclusive, option is that foreign antigens or superantigens, from chronic viral or recurrent bacterial infections, could be at the root of selection, and 2 types of stimuli (self- and non–self-antigens) might act concomitantly or sequentially during leukemogenesis. Many other possibilities can be envisioned: for example, lesions allowing more effective signaling through the BCR and other pathways; greater sensitivity to cytokine or chemokine encounters; more effective trafficking to anatomic sites where survival signals could be received; and so on. Additional, complementary DNA aberrations, not necessarily the same in all patients, would follow promoting activities with eventually a final abnormality, which seals the leukemic fate, occurring in predisposed cells.
Possibilities for the cellular origin of CLL
Because the precise stage of B-cell differentiation at which the final transforming event occurs may be imposed by promoting activities, a stepwise, longitudinal model would permit CLL derivation from either a single or multiple B-cell subsets. If the cell of origin is singular, then the final genetic event leading to full-blown CLL would probably be restricted to either a unique B-cell lineage or a specific stage of B-cell maturation. However, if multiple cell types give rise to distinct subgroups of CLL, a longitudinal model would suggest that leukemic cells with one or more transforming lesions proceed along normal B-lymphocyte maturation steps, with the final transformation occurring in one of several B-cell subsets (Figure 1), arising randomly or specifically, based on the promoting factor delivered or time of deliverance. The B-cell subset in which the final abnormality occurs would dictate many of the structural and functional features of the leukemia, although it would not indicate that all of the genetic abnormalities leading to malignancy occurred at this stage. At this point, the fully transformed clone with a growth advantage would become predominant over others still “blocked” at earlier pretransformation stages.
In either case, we return to the pivotal conundrum. How can we reconcile clear differences among patients in BCR stereotypy and autoantigen binding, which associate with IGHV mutation subgroups, with gene expression data suggesting a single precursor? Could the activated phenotype found in all CLL cases obscure inherent B-cell subset gene expression differences between distinct precursors of U-CLL and M-CLL? If the transformation process is identical for both U-CLL and M-CLL, could relatively similar gene expression profiles reflect a common “CLL-related” gene expression phenotype, regardless of the cell type transformed? Finally, can differences in expression of approximately 20 to 100 genes reflect different B-cell lineages, especially if both B-cell subtypes were activated in some manner? In this regard, it is important to consider that only 4 genes control the differentiation program of mature cells.139,140 If one accepts the possibility of an alternative interpretation of gene expression profiles of CLL cells, a multiple cell model, involving several B-cell types, is feasible.
Although the accumulated data do not provide definitive normal counterpart(s) in CLL, they provide a framework to build hypotheses and frame further studies. In this spirit, we offer the following possibilities as straw men models to improve on to yield definitive answers.
First, regardless of the number of precursors, we propose that CLL cells have cycled before complete transformation, in some cases quite significantly, presumably influenced at least in part by BCR-antigen interactions. Thus, we expect the normal counterpart to be an antigen-experienced B cell, although the stage at which this experience began could vary and encompass any stage of B-cell maturation after the expression of a rearranged IGH (Figure 1A). This is consistent with the most recent World Health Organization classification of tumors of hematopoietic and lymphoid tissues,141 denoting CLL as a neoplasia of antigen-experienced B cells.
Second, if there is a single normal counterpart for CLL, we think that the final transforming event in a stepwise transformation process would most probably occur in an MZ B cell, a transitional B-cell, or a human B-1-like cell. We favor the MZ population giving rise to both U-CLL and M-CLL because these cells display more of the key features of CLL cells. MZ B lymphocytes respond to T-independent and T-dependent antigens and can display activated membrane phenotypes after antigen encounter. In addition, they express BCRs coded by unmutated or mutated IGV genes,28 which are polyreactive as well as autoreactive81,142 and, in some instances, are capable of providing innate protection against microbes. The main disclaimer for an MZ origin of CLLs is the difference in cell surface phenotype, although this difference could reflect the activated state of CLL cells. A human B-1 cell equivalent also might give rise to CLL. Like MZ B cells, these cells usually use unmutated IGV to code for polyreactive and autoreactive Igs, which can serve as protectors from microbes and as eliminators of catabolic debris. In addition, B-1 cells can give rise to a CLL-like disease in aging mice.143 The lack of an identified human counterpart and the near exclusion of IGV mutations in this population in mice create major difficulties in choosing B-1 cells as progenitor of all CLL clones. However, recently B-1 cells from aged mice were found to exhibit some IGV gene features of follicular B lymphocytes (N-region additions), although V-region mutations were not analyzed.144 Furthermore, Ig class switching can occur in B-1 cells,78 a process controlled by AID,145-148 like IGV somatic mutations. If a B-1 cell counterpart does not exist in humans, its function may have been assumed by an MZ subset.149,150 Finally, transitional B cells151 might serve as precursors of all CLL cells because they express CD5,152,153 can be autoreactive,154 and surprisingly express both unmutated and mutated BCRs, presumably because they can express AID, at least in mice. Furthermore, normal immature B cells from sheep,155 mice,146,156 and rarely humans157,158 can exhibit mutated IGVs. Of interest, there may be a direct developmental pathway in mice from transitional to MZ B cells.150,159 The findings against transitional B lymphocytes as the single source of CLL are expression of CD10, not seen on CLL cells unless undergoing apoptosis,160 absence of CD27, which is consistently found on CLL cells, and lack of responsiveness to BAFF/BLyS/TALL-1,152 which very effectively supports CLL cell survival.
Lastly, all these same populations could be sources of U-CLL if there are multiple cells evolving into CLLs. For example, B-1 cells in mice can display stereotyped BCRs, and transitional B cells and MZ B cells can express unmutated autoreactive receptors. Therefore, in a multiple normal counterpart model of CLL, we favor a human B-1 cell equivalent giving rise to U-CLL with polyreactive BCRs, particularly those exhibiting stereotypy, and transitional and/or MZ B cells as a source for U-CLL without stereotypy. In a multiple model, we suggest that M-CLLs derive from transformation of MZ and/or post-GC memory B cells. A post-GC origin is supported by the occurrence in some M-CLL clones of mutated bcl-6, a gene used by and needed for GC formation.126 bcl-6 with a similar pattern of mutations is used by normal post-GC memory B (not virgin B cells) in proportions similar to that of M-CLL clones,161,162 as well as in IgMhighIgDlowCD27+ B cells,33 which may be of MZ origin. AID-expressing transitional B cells could also be M-CLL precursors in a multiple cell model because these cells might express mutated as well as unmutated BCRs.
Conclusions
Most of our knowledge about CLL cells derives from studying circulating cells, not those residing in solid lymphoid tissues. Although certain findings would not be affected by this fact, for example, IGV gene use, assembly, and mutations as well as Ig binding specificity, others, such as gene expression, would be, as recently documented.163 CLL cells most probably proliferate and expand because of protection from apoptosis in proliferation centers of lymphoid tissues and bone marrow. Once they leave these areas and reach the circulation, these cells could become progressively less robust, developing an enhanced propensity to apoptose. CLL cells in proliferation centers could be viewed as composing a “proliferative compartment,” progeny of “stem-like cells,” whereas those in the blood are less robust cells, which could again be recruited into the proliferating fraction, should they make their way to solid tissues and encounter appropriate environmental conditions and accessory signals. These re-entering cells could be considered part of a “resting/re-entry compartment.” This life cycle is in line with in vivo kinetic studies demonstrating both active proliferation and disappearance of CLL cells.6,164,165 Corroborating this view are the progressive shortening of telomeres and up-regulation of telomerase in CLL cells5,166 and the self-renewing capacities of murine B-1 cells,76 should these cells be progenitors of all or of certain subtypes of CLL cells.
Although it is possible that every CLL could be stem-like, as in the scenario in the preceding paragraph, the existence of a true CLL stem cell that developed, somatically, self-renewing capacities is also plausible.167 Indeed, the concept of a stepwise evolution to leukemia opens the possibility that precursors of CLL exist to serve as reservoirs from which flow maturing leukemic cells that fill the leukemic bulk in the periphery. Such a cell could be positioned at any B-cell differentiation stage after IGV rearrangement at both the H- and L-chain loci (Figure 1). Of note, mRNA transcripts coding for CLL-specific IGHV/D/J rearrangements have been found in preswitch B cells from IgG-expressing CLL patients.168 Furthermore, differentiation of CLL cells into Ig-secreting plasma cells can arise spontaneously in vivo169,170 and be induced in vitro.171,172 Such CLL stem cells would occupy sustaining and protective niches in lymphoid tissues and proliferate when appropriate stimuli are delivered. Because of the requirement for a functioning BCR and of constraints on BCR structure and specificity imposed by clonal development, this stem cell should not be too distant in the maturation pathway from most CLL cells in the clone. Although BCR-antigen interactions could lead to maturation of this stem cell to a mature CLL cell, smIg need not exist constitutively on these progenitors but could be induced. Nevertheless, expression of surface BCRs on such cells would eventually occur and be advantageous, as identical changes in BCR structure occur infrequently in a large number of CLL subclones173 ; and when they do occur, they tend to preserve the antigen-binding site and suggest antigen selection.174,175 Thus, the degree of maturation of CLL stem cells could be limited, differing from myeloproliferative disorders.176
Finally, although the CLL research community has not yet solved the issue of the cell of origin of CLL, the problem has been more precisely defined, and new possibilities, such as stepwise clonal evolution, defined. Our aim in this Perspective has been to outline some of the problems and to provide a framework into which novel data can be inserted. We end by suggesting problems that remain to be addressed.
Because our understanding of B-cell biology in humans is not as robust as in mice, a more complete definition and characterization of all human B-cell subsets are essential. In particular, the human B-1 cell equivalent should be sought in different anatomic sites, using cellular and molecular biology methodologies. Furthermore, a more precise definition of IGV gene use and assembly within human B-cell subsets is crucial, as it could elucidate progenitor-effector cell relationships between normal and leukemia/lymphoma cells and further clarify the role of antigen stimulation and selection before, during, and perhaps after full-blown transformation. Finally, an analysis of initial and ongoing DNA and methylation alternations and their consequences on gene expression within various B-cell subsets during the course of activation may lead to clarification of some of the problems mentioned, in particular the existence of CLL-specific signatures that might be distinguishable from B-cell activation signatures. Because technologies to address these questions are becoming available at an amazingly rapid rate, it is probable that such information will be available soon.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank the members of the Karches Center for CLL Research, the Feinstein Institute for Medical Research, North Shore-LIJ Health System, and the Division of Medical Oncology C, Istituto Nazionale per la Ricerca sul Cancro for discussions on this work.
This work was supported in part by the National Cancer Institute (RO1 grant CA81554), the National Center for Research Resources (M01 General Clinical Research Center grant RR018535), the Associazione Italiana Ricerca sul Cancro, Ministero dell'Istruzione dell'Universitá e della Ricerca, Fondazione San Paolo, Ministero Salute 2006, the Karches Foundation, the Prince Family Foundation, the Marks Foundation, the Jerome Levy Foundation, the Leon Levy Foundation, the Tebil Foundation, Inc, and the Joseph Eletto Leukemia Research Fund.
National Institutes of Health
Authorship
Contribution: N.C. and M.F. synthesized ideas and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Nicholas Chiorazzi, Feinstein Institute for Medical Research, 350 Community Dr, Manhasset, NY 11030; e-mail: NChizzi@NSHS.edu; or Manlio Ferrarini, Istituto Nazionale per la Ricerca sul Cancro, Largo Rosanna Benzi, n. 10, 16132 Genova, Italy; e-mail: Manlio.Ferrarini@ISTGE.it.