The capacity of saliva to clot blood has been documented in the scriptures (Luke 16:21), folklore, and in the medical literature of the 1920s when Hunter described the ability of saliva to clot blood and proposed it as a means to attenuate bleeding from gastric ulcers.1 In 1938, Glazko and Greenberg reported that saliva contains a cell-derived, protein-based thromboplastin,2 which was later identified as tissue factor.
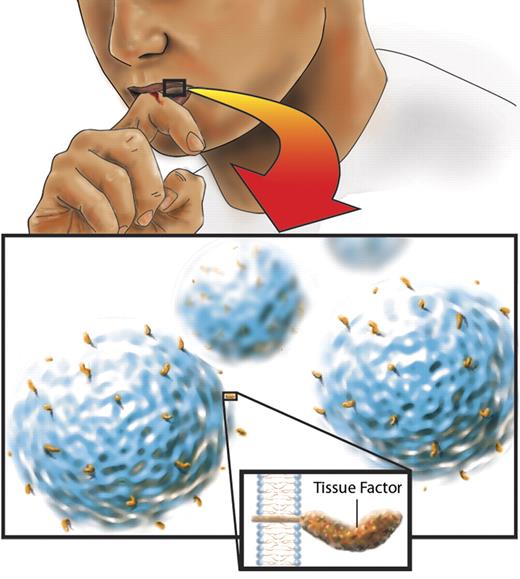
Where is the source of tissue factor in saliva? In 1979, Zacharski and Rosenstein reported that almost one-quarter of the tissue factor procoagulant activity in saliva remains in the supernatant after centrifugation of the cells.3 Using contemporary techniques, Berckmans and colleagues have now identified the source of the tissue factor procoagulant activity in the supernatant.4 Salivary tissue factor is associated with microvesicles and exosomes. These are vesicles that are shed from cells.5 Shedding occurs in resting cells, but increases with cell stimulation or apoptosis. The tissue factor–bearing vesicles in saliva are likely derived from cells in the salivary glands and the mouth because they express epithelial-cell and leukocyte markers on their surface (see figure). The concentration of tissue factor in these vesicles is at least 5-fold higher than that in blood, so there is more than enough to clot blood!6
Tissue factor on microvesicles in saliva can cause blood to clot. This may provide the basis for the wound-licking reflex. Illustration by Nima Vaezzadeh.
Tissue factor on microvesicles in saliva can cause blood to clot. This may provide the basis for the wound-licking reflex. Illustration by Nima Vaezzadeh.
In this issue of Blood, Berckmans et al suggest that salivary tissue factor serves as an extra barrier between the blood and the outside milieu by promoting hemostasis and preventing infection. Blood pools in the saliva when the oral mucosa is injured. In the absence of flow, only low concentrations of tissue factor are required to trigger thrombin generation,7 provided that there are an adequate number of normal platelets.8 Could this explain, at least in part, why oral mucosal bleeding is more common with platelet disorders than with deficiencies of clotting factors?
As with all science, answers beget more questions. In mice, removal of the salivary glands decreases wound healing.9 Is the poor wound healing the result of an absence of salivary tissue factor? Do the levels of salivary tissue factor change with aging or disease? Would strategies aimed at increasing salivary tissue factor reduce mucosal bleeding in patients with thrombocytopenia or gingivitis, or even those with gastric ulcers? These are questions for the future. Meanwhile, the work by Berckmans and colleagues provides some basis for why the wound-licking reflex may be beneficial. The clot-promoting activity of saliva may be offset by harm, including the introduction of oral bacteria into the wound.10
Conflict-of-interest disclosure: The author declares no competing financial interests. ■