Abstract
Accumulating evidence has designated B cells as central players in the pathogenesis of immune diseases. In the late 1990s, anti-CD20 monoclonal antibodies were developed for the treatment of B-cell non-Hodgkin lymphomas, offering the opportunity to efficiently deplete the B-cell compartment for therapeutic immunointerventions. Several studies have since established the beneficial effect of this drug on the course of a wide range of immune diseases. However, paradoxically, it has also been reported that rituximab sometimes worsens the symptoms of the very same conditions. The explanation that reconciles such apparently conflicting results has recently emerged from basic studies, which demonstrate that (1) B cells are also endowed with immune-regulatory properties and (2) the opposing contributions of B cells may overlap during the course of the disease. Caution should therefore be exercised when considering B-cell depletion because the therapeutic effect will depend on the relative contributions of the opposing B-cell activities at the time of the drug administration.
“Bad boy” B cells
Historically, the role of B lymphocytes in the pathogenesis of immune diseases has been associated mainly with their capacity to produce harmful antibodies after differentiation into plasma cells. This conception was based on seminal experiments that demonstrated that the mere transfer of antibodies was sufficient to recapitulate the symptoms of myasthenia gravis, Graves disease, Goodpasture disease, among others.1 In contrast to these diseases, other autoimmune conditions, in which the role of antibodies has not been recognized, have traditionally been termed “T cell–mediated” diseases. Among the latter, type 1 diabetes, in which T lymphocytes are crucial for the destruction of the β islets, has long been considered as archetypal. However, recent investigations in nonobese diabetic mice have shown that more than 50%2 of the lymphocytes infiltrating islets of Langerhans are B cells3 and that these B cells are critically necessary for the development of diabetes.4 Another clue that B cells exert pathogenic roles through “antibody-independent” mechanistic pathways came from genetically modified lupus-prone mice. Although B-cell depletion leads to abrogation of the disease in this model, transgenic mice, whose B cells cannot secrete immunoglobulin, still developed nephritis.5 Thus, in many immune diseases, even including those not driven by antibodies, B cells have been demonstrated to play an essential pathogenic role.
Among the antibody-independent pathogenic roles of B cells, accumulating evidence points to their capacity to present antigen.6 Upon recognition of specific antigen, the B-cell membrane is reorganized resulting in the aggregation of B-cell receptor in an immunologic synapse that functions as a platform for internalization of the complex.7 Internalized antigen is degraded and subsequently exposed on the B-cell surface in association with major histocompatibility complex molecules for presentation to T cells. This surface presentation of antigen, in the presence of various costimulatory molecules, elicits the T-cell assistance required for B-cell maturation, which in turn allows B cells to drive optimal T-cell activation and differentiation into memory subsets8 (Figure 1 left panel). Of note, B cells are endowed with unique properties as antigen-presenting cells because they have an antigen-specific receptor, allowing extraction and presentation of antigen, even if it is membrane tethered9 or present in limiting quantities.10 Furthermore, B cells also have the capacity to clonally expand, thereby becoming the numerically dominant antigen-presenting cells.
Janus-faced B cells. Janus, the Roman god of beginnings and endings, is most often depicted as having 2 faces facing opposite directions. Like him, B cells can either elicit (right panel) or terminate (left panel) an immune response, after their activation by combination of ligation of the B-cell receptor, CD40, and Toll-like receptors (TLRs). (Left panel) B cells present the antigen along with costimulatory signals, leading to the activation and the proliferation of T effectors. In turn, activated T cells provide CD40 ligand (CD40L) for the differentiation of B cells into antibody-producing plasma cells. The cytokines produced by B cells may participate into the polarization of T effectors. Finally, B cells play a critical role for the development of T-cell memory. (Right panel) B cells regulate immune response by provision of IL10 that suppresses the activation and the expansion of T effectors directly, and indirectly through the differentiation of T regulatory cells and the suppression of dendritic cell function.
Janus-faced B cells. Janus, the Roman god of beginnings and endings, is most often depicted as having 2 faces facing opposite directions. Like him, B cells can either elicit (right panel) or terminate (left panel) an immune response, after their activation by combination of ligation of the B-cell receptor, CD40, and Toll-like receptors (TLRs). (Left panel) B cells present the antigen along with costimulatory signals, leading to the activation and the proliferation of T effectors. In turn, activated T cells provide CD40 ligand (CD40L) for the differentiation of B cells into antibody-producing plasma cells. The cytokines produced by B cells may participate into the polarization of T effectors. Finally, B cells play a critical role for the development of T-cell memory. (Right panel) B cells regulate immune response by provision of IL10 that suppresses the activation and the expansion of T effectors directly, and indirectly through the differentiation of T regulatory cells and the suppression of dendritic cell function.
In addition to antigen presentation, activated B cells also produce a wide range of cytokines and chemokines that modulate the maturation, migration, and function of other immune effectors.11,12 In particular, B cells have been shown to play a critical role in lymphoid neogenesis,13 that is, the process by which ectopic functional lymphoid structures (“tertiary lymphoid tissues”) appear de novo during chronic inflammation.14,15 Several studies16-18 have demonstrated that tertiary lymphoid tissues are permissive microenvironments for the induction of immune responses and have led to the hypothesis that lymphoid neogenesis may contribute to the exacerbation of a wide range of chronic inflammatory diseases.19
Anti-CD20 monoclonal antibody for therapeutic B-cell depletion
Given the multiple pathogenic roles attributed to B lymphocytes, therapeutic strategies that aim at depleting this cell population were expected to be beneficial in a wide range of immune diseases.
Pioneer attempts to deplete B cells in the 1980s relied on xenogenic polyclonal antibodies directed against the surface immunoglobulin receptor.20 Finally, it was only in the late 1990s that progress achieved in the treatment of lymphoproliferative disorders offered clinicians the opportunity to efficiently target the B-cell compartment for therapeutic immunointerventions.
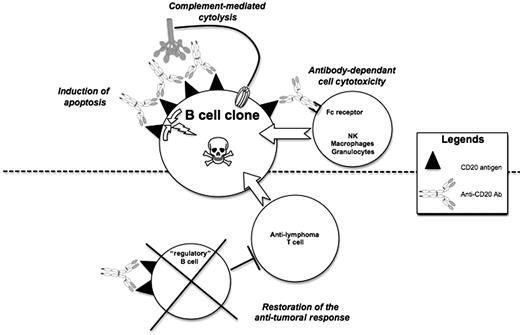
CD20 is a transmembrane protein that functions as a Ca-permeable cation channel, whose expression is restricted to B cells from the pre-B-cell to the immunoblast stage.21 Rituximab, a chimeric monoclonal antibody composed of human immunoglobulin G1 kappa antibody with variable regions isolated from a murine anti-CD20 clone (IDEC-2B8),22 was initially introduced for the treatment of B-cell non-Hodgkin lymphomas.23 A single course of rituximab successfully depleted peripheral human B lymphocytes for periods ranging from 3 months to more than 1 year through mechanisms involving Fc- and complement-dependent killing as well as other signals inducing apoptosis24 (Figure 2 top panel). Several studies have highlighted the influence of circulatory dynamics and microenvironment on the efficiency of rituximab depletion.25,26 As a result, the reduction of B-cell numbers after rituximab appears to be less complete in secondary lymphoid tissues than in peripheral blood, and variations in the extent and kinetics of the depletion have been reported among B-cell subsets.1
Mechanisms of action of anti-CD20 antibodies. (Top panel) Apoptosis of malignant B-cell clones occurs upon cross-linking of rituximab-CD20 complexes in the lipid rafts. This activates signaling pathways involving the Src kinases and their regulatory molecules. Complement-mediated cytolysis involves the ability of anti-CD20 immunoglobulin G1 bound to their antigen to bind C1 and trigger the classical complement pathway. Antibody-dependent cell cytotoxicity requires interaction between the Fc portion of rituximab and appropriate receptors on effector cells. (Bottom panel) Another possible mechanism by which rituximab could promote the destruction of malignant B-cell clones is the restoration of the protective antitumoral response. The destruction of the nonmalignant B cells endowed with immune-regulatory properties could facilitate the development of antitumoral T-cell clones.
Mechanisms of action of anti-CD20 antibodies. (Top panel) Apoptosis of malignant B-cell clones occurs upon cross-linking of rituximab-CD20 complexes in the lipid rafts. This activates signaling pathways involving the Src kinases and their regulatory molecules. Complement-mediated cytolysis involves the ability of anti-CD20 immunoglobulin G1 bound to their antigen to bind C1 and trigger the classical complement pathway. Antibody-dependent cell cytotoxicity requires interaction between the Fc portion of rituximab and appropriate receptors on effector cells. (Bottom panel) Another possible mechanism by which rituximab could promote the destruction of malignant B-cell clones is the restoration of the protective antitumoral response. The destruction of the nonmalignant B cells endowed with immune-regulatory properties could facilitate the development of antitumoral T-cell clones.
Successes of therapeutic B-cell depletion
The most frequent hematologic malignancy is non-Hodgkin lymphoma, 85% of which are of B-cell origin. Rituximab has been approved for the treatment of B-cell non-Hodgkin lymphoma in 1997. Since then, several randomized, phase 3 trials have reported significant survival benefits associated with rituximab, in combination with chemotherapy, in patients with diffuse large B-cell lymphoma and follicular lymphoma. Furthermore, these benefits have been demonstrated for rituximab in combination with a wide variety of chemotherapy regimens, across many patient subtypes, and in different treatment and disease settings (for a recent review please see Hagemeister27 ), leading to the conclusion that anti-CD20 monoclonal antibodies represent one of the most important advance in the treatment of B-cell lymphoma in the past 30 years.
In chronic lymphocytic leukemia, the leukemic counterpart of small lymphocytic lymphoma, the addition of rituximab to fludarabine-based chemotherapy has significantly increased complete response and progression-free survival rates for both untreated and relapsed or refractory chronic lymphocytic leukemia.27
The association between autoimmune diseases and hematologic malignancies has long been recognized. Although autoimmune conditions associated with hematologic malignancies can affect any organ, they seem to predominantly target blood constituents.28 The pathophysiology of these autoimmune manifestations is complex and remains incompletely understood. Autoimmune anemia, for example, either can result from monoclonal antibodies produced by the lymphoma clone (ie, cold hemagglutinin disease) or can be the consequence of polyclonal autoantibodies produced by the residual nonmalignant B cells in chronic lymphocytic leukemia. Several reports suggest that treatments, in particular chlorambucil and fludarabine, might trigger the onset of autoimmune manifestations.29,30 In contrast, rituximab has been shown to be an effective treatment for chronic lymphocytic leukemia–associated autoimmune hemolytic anemia,28,31 and for mixed cryoglobulinemia and cold agglutinins secondary to non-Hodgkin lymphoma.32
These observations along with the favorable safety profile of the rituximab in patients treated for hematologic malignancies33 have catalyzed the application of the drug in primary immune diseases. Several clinical studies have since established the beneficial effect of B-cell depletion on the course of a wide range of immune diseases.
Rheumatoid arthritis, a multisystem disorder that predominantly causes inflammation in synovial joints, is the autoimmune condition in which the effect of rituximab has been the most studied.34 In the pivotal phase 2a study, approximately 80% of patients with active rheumatoid arthritis (despite methotrexate treatment) showed clinical benefit after rituximab administration—a percentage similar to the one obtained with anti–tumor necrosis factor agents.35 Furthermore, a recent phase 3 trial has reported that even patients with an inadequate response to anti–tumor necrosis factor agents showed significant improvement after rituximab therapy,36 a result that prompted the Food and Drug Administration to approve the drug for the treatment of refractory rheumatoid arthritis.
In chronic idiopathic thrombocytopenic purpura, an acquired hemorrhagic condition associated with accelerated platelet consumption due to antiplatelet autoantibodies, a phase 2 study has reported a 40% good response rate to rituximab.37
Based on previous encouraging case reports, a phase 2 controlled clinical trial has recently been conducted in multiple sclerosis. In patients with relapsing-remitting multiple sclerosis, a single course of rituximab reduced inflammatory brain lesions and clinical relapses for 48 weeks.38
Numerous small, open-label studies and isolated cases have also reported favorable outcomes after rituximab administration in a wide range of autoimmune diseases, including vasculitis,39 autoantibody-associated neuropathies,40 Graves disease,41 myasthenia gravis,42 myositis,43 blistering skin disorders,44,45 mixed cryoglobulinemia,46 thrombotic thrombocytopenic purpura,47 Sjögren syndrome,48 and anti–factor VIII syndrome.49 There are ongoing phase 2 and 3 trials of rituximab for each of these autoimmune disorders.50
Finally, recent advances in solid organ transplantation have unraveled new mechanisms of allograft damage. Unexpected clusters of CD20+ B cells have been discovered in rejected grafts,18,51 and C4d deposition, indicating classic complement pathway activation, is now routinely seen in refractory rejection.52 Rituximab has therefore emerged as a rational choice for therapy in transplantation to abrogate B cell–mediated events.53,54
Limits of therapeutic B-cell depletion
Given the central role of B cells, autoantibodies, and immune complexes in the pathophysiology of systemic lupus erythematosus (SLE), it was widely anticipated that anti-CD20 would be efficient in treating SLE. However, despite the successes reported in some open-label preliminary studies,55,56 rituximab failed to meet its primary and secondary end points in 2 large controlled trials of nonrenal SLE57 and renal lupus nephritis.58 These disappointing results are sometimes attributed to the fact that the highly heterogeneous clinical presentation of SLE makes it difficult to devise quantitative measures of response to therapy. However, the latter justification is an unlikely explanation for either the paradoxical exacerbation of the clinical condition59-61 or the onset of new immune diseases (including psoriasis,62,63 vasculitis,64-66 interstitial pneumonitis,67-69 and autoimmune cytopenia70,71 ) that are sometimes observed after rituximab administration. One could argue that these small nonrandomized studies focus on a very rare adverse effect of rituximab, because this problem was not identified in the huge cohort of patients treated for hematologic malignancies.33 We rather favor the alternative explanation that rituximab-induced autoimmune complications are underreported. It is indeed a well-established fact that the quality and quantity of drug safety reporting are inadequate,72 a matter that seems even more common for drugs with excellent efficacy outcomes.72 One can indeed conceive the reluctance of clinicians to report side effects of a drug that has changed the standard of care for patients suffering from life-threatening diseases such as non-Hodgkin lymphoma or chronic lymphocytic leukemia. Furthermore, the widely recognized association between autoimmune diseases and hematologic malignancies already discussed makes very difficult the formal incrimination of the drug for these patients. The same concern also exists for patients receiving rituximab for an autoimmune disease, the occurrence of distinct autoimmune conditions in the same patients being a very common feature.73 Thus, the current lack of a consistent demonstration of the increased incidence of autoimmune phenomena after rituximab administration does not exclude the possibility that a carefully conducted meta-analysis might still be able to detect this adverse event.
In this context, the results of the study recently published by Clatworthy et al74 are particularly interesting because they clearly establish the “paradoxical” immune stimulatory effect of rituximab. Indeed, this randomized controlled trial, which compared rituximab with an anti-CD25 monoclonal antibody as induction therapy in patients undergoing renal transplantation, had to be suspended because the authors observed a 6-fold increased incidence of acute cellular rejection in the rituximab group (83% vs 14%).
Based on the worsening of autoimmunity observed in chronic lymphocytic leukemia patients receiving fludarabine,29,30 a drug that induces a profound lymphopenia, it is tempting to speculate that this paradoxical immune stimulation is rather a general feature after B-cell depletion than a specific adverse effect of rituximab.
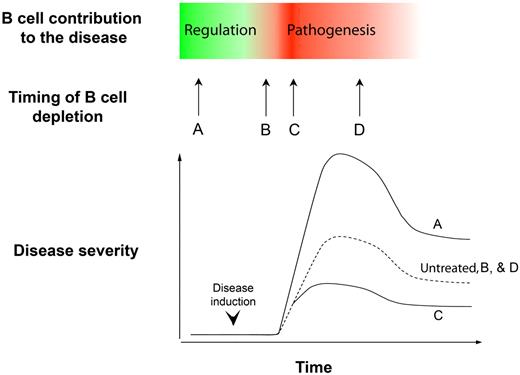
Finally, the ambivalence of B-cell depletion on the course of immune diseases has been recently demonstrated in experimental autoimmune encephalomyelitis.75 Experimental autoimmune encephalomyelitis (EAE) is an autoimmune central nervous system disease that can be induced in certain susceptible murine strains after immunization with myelin to model human multiple sclerosis. Whereas CD20 antibody–mediated B-cell depletion during EAE disease progression dramatically reduced the symptoms, the same treatment given before EAE induction substantially exacerbated the disease (Figure 3). Interestingly, administration of the drug at other time points had no significant effect (Figure 3).
B-cell depletion has ambivalent effects on the course of immune diseases. The figure is a schematic representation of the findings of Matsushita et al.75 During the course of EAE, B cells play opposite overlapping roles. Depending on the timing of anti-CD20 antibody administration, the net clinical effect can be deleterious, neutral, or beneficial. Dashed lines indicate the severity of EAE in untreated control animals.
B-cell depletion has ambivalent effects on the course of immune diseases. The figure is a schematic representation of the findings of Matsushita et al.75 During the course of EAE, B cells play opposite overlapping roles. Depending on the timing of anti-CD20 antibody administration, the net clinical effect can be deleterious, neutral, or beneficial. Dashed lines indicate the severity of EAE in untreated control animals.
Altogether, these data demonstrate that it is more difficult than anticipated to forecast the effect of B-cell depletion on the course of an immune disease: the same therapy can lead to opposite outcomes depending on the timing of its administration.65
Evidence for an immune-regulatory role of B cells
The explanation that reconciles such apparently conflicting results has recently emerged from basic studies that demonstrate an immune-regulatory role of B cells.
The first clue that B cells can regulate immune responses was provided by seminal in vivo experimental studies by Shimamura et al, demonstrating that adoptive transfer of antigen-activated B cells could induce tolerance in naive mice through the induction of suppressor T cells.76 Despite these data, the role of B cells in the regulation of immune diseases remained overlooked for another decade, until Wolf et al reported that mice lacking B cells suffered an unusually severe and chronic form of EAE.77 Although spontaneous recovery is the norm in wild-type mice, the authors observed that genetically B cell–deficient mice of the same background experienced a greater variation in disease onset and severity, and failed to recover completely. After this seminal contribution, independent groups made consistent observations in other experimental models of autoimmune diseases, including collagen-induced arthritis78 and a model of spontaneous colitis, pathologically reminiscent of human ulcerative colitis.79 Interestingly, whereas the pathogenic T-cell response involves the same T helper 1 (Th1) cells and Th17 proinflammatory T-cell populations in EAE and collagen-induced arthritis, the colitis model differs in that the inflammation appears to be driven by Th2 cells. Thus the B-cell compartment has the capacity to control organ-specific inflammation that may be driven by Th1, Th2, or Th17 effectors.
Dissection of the underlying mechanisms revealed that B cells limit immune disease progression by providing interleukin-10 (IL-10)75,78,80-82 that, in turn, directly suppresses the differentiation of pathogenic T cells, promotes the development of regulatory T cells,83 and constrains dendritic cell functions84 (Figure 1 right panel).
Which B cells control the immune responses?
B cells can be stimulated to produce IL-10 by a combination of ligation of the B-cell receptor by the antigen and of CD40 by CD40 ligand. Some reports also point to a critical nonredundant role of certain Toll-like receptors (TLR2 and TLR4) in driving the regulatory activity in B cells.87
The involvement of the B-cell receptor, CD40, and TLRs in the regulatory function of B cells raises a conceptual difficulty. Indeed, these signals are the very same as the ones involved in the activation of B cells in most immune responses. One hypothesis would therefore be the existence of a peculiar “B-reg” subset, endowed with the unique function to regulate immune processes. In the mouse, B cells are classically divided into B-1 cells that reside in pleural and peritoneal cavities and B-2 cells that populate secondary lymphoid organs. Peritoneal B-1 cells, known to produce particularly large amounts of IL10 after stimulation, have been ascribed with regulatory function in some studies.88,89 However, because this subset was excluded from the transfer experiments demonstrating the regulatory role of B cells,78,80,90 it is likely that B-2 cells also contain a subset regulating immune diseases.
Interestingly, a rare population of splenic B cells characterized by a unique phenotype that associates features from B-1 (expression of CD5) and B-2 (high expression of CD1d, like the marginal zone B cells) cells has recently been reported to play a critical role in the regulation of murine EAE.82 However, the B-cell subsets involved in suppression of other experimental immune diseases do not have exactly the same phenotype.81,91-94
Ambiguity therefore remains regarding the B-cell subpopulation(s) involved in the regulation of immune responses. An alternative hypothesis is that the immune-suppressive activity is not a unique property of a single B-cell subset but is perhaps exerted by different B-cell subsets, depending on the integration of available signals in the microenvironment.
Clinical implications
Collectively, these studies demonstrate that Janus-faced B cells play both pathogenic and regulatory activities in immunopathogenesis (Figure 1) and that these opposing contributions may overlap during the course of the disease. Consequently, the therapeutic effect of B-cell depletion depends on the relative contributions of the opposing B-cell activities at the time of drug administration (Figure 3). It would be of utmost importance to define simple criteria or reliable markers that would help to predict whether administration of rituximab would be beneficial for the patient. Although there are clues about directions that should be taken in the future, there is no easy answer to this question yet. The recent identification of a human B-cell subset with regulatory properties in the peripheral blood of lupus patients86 represents an important step but will likely be insufficient because this subset appears to be qualitatively rather than quantitatively deficient in these patients.86 A functional assay, which would measure the response of T cells to a normalized stimulation in presence or absence of the B cells, could be theoretically useful but its development would require an important amount of work, the limitations of functional assay for routine immunomonitoring being well known (minor changes of test conditions potentially having a major impact on the test results, necessity to work with freshly isolated cells, etc).
Of note, immune stimulation resulting from the removal of B-cell regulation could also be used in a therapeutic perspective. This strategy could be particularly useful in cancer, where B cells have been shown to inhibit the induction of T cell–dependent protective antitumor immunity.95 Accordingly, the administration of anti-CD20 antibodies slowed the growth of nonhematopoietic solid tumors (not expressing CD20) and enhanced the efficiency of a tumor vaccine in a murine model.96 It is thus conceivable that the mode of action of rituximab in hematologic malignancies also relies in part on such a mechanism (Figure 2 bottom panel).
Conclusions
The optimization of B-cell depletion strategies for the treatment of immune diseases therefore not only should focus on the identification of new targets and the development of more depleting drugs, but also requires a better understanding of the complex temporal interplay between pathogenic and regulatory B cells. Instead of a mere depletion of the B-cell compartment, future therapy should instead attempt to reset the regulatory balance—to which B cells can clearly contribute.
Acknowledgments
This work was supported by grants from the CENTAURE Transplantation Research Network and the Hospices Civils de Lyon.
Authorship
Contribution: O.T., E.M., and T.D. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Olivier Thaunat, Service de Transplantation Rénale et d'Immunologie Clinique, Hôpital Edouard Herriot, 5 place d'Arsonval, 69437 Lyon Cedex 03, France; e-mail: olivier.thaunatpastu@free.fr.