Abstract
Abstract 855
Despite its often indolent clinical course, follicular lymphoma (FL) is a heterogeneous disease. Current criteria for early identification of patients with a poor prognosis are suboptimal - the FLIPI and F2 index are insufficient prognostic markers for individual patients and the limitations of post-treatment conventional response criteria have long been acknowledged. FL shows increased FDG uptake, but unlike DLBCL, minimal data exist about the role of PET-CT in response assessment. We have used the prospective conventional response assessment and 42 month patient follow-up in the PRIMA (Primary Rituximab and Maintenance, Salles et al., ASCO 2010, Abstr#8004) study as a platform for analysis of the utility of PET-CT in FL.
The PRIMA database was interrogated and investigators surveyed to identify PET-CT scans performed during staging and induction response assessment. Single modality PET-only scans were not eligible for inclusion. Local PET interpretation (positive + or negative -) was used to explore associations with patient outcomes. The primary endpoint was PFS from PRIMA registration.
277 PET-CT scans on 160 patients from 40 centres were identified. Baseline patient characteristics did not differ from the overall PRIMA patient population. Positive PET-CT scans were recorded in 119/120 (99%) at diagnosis, 11/33 (33%) interim restaging scans and 32/124 (26%) post induction treatment (R-CHOP or R-CVP).
There was significant correlation between PET-CT result and conventional response assessment at the end of immunochemotherapy (p<0.0005). The incidence of post-treatment PET+ increased across the categories of lesser conventional responses, occurring in 8% (4/50) CR, 31% (12/39) CRu, 41% (11/37) PR, 67% (2/3) SD, and 80% (4/5) PD. While 73/91 (80%) of PET- patients were in CR/CRu, given the very high overall response rate on study, 16/33 (48%) of the PET+ population were also in CR/CRu.
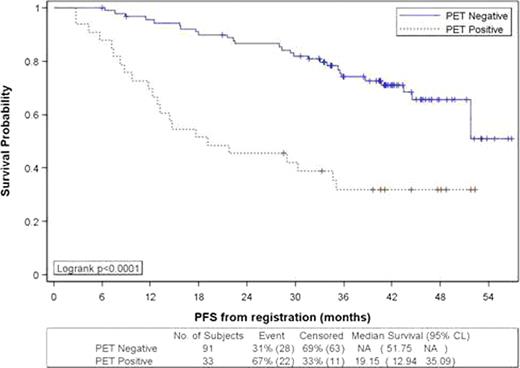
With a median follow-up of 42 months, a significantly inferior actuarial 3yr PFS was observed in post-treatment PET+ vs. PET- patients (Figure 1): 32% (95% CI 17–48%) vs. 74% (95% CI 63–82%) (log rank p<0.0001, HR 3.5, 95% CI 2.0–6.1), median PFS 19 months (13-35) vs. not reached, (52-NR).
Using proportional hazard regression analysis, both conventional response (overall p=0.0002) and PET+ status (HR 2.8 p=0.0007) were significant predictors of inferior PFS. However, the predictive power of conventional response assessment was limited to non-responders: SD/PD vs. CR/CRu (HR 6.5, p<0.0001), and SD/PD vs. PR (HR 5.2, p=0.0009). Comparison of PR vs. CR/CRu was not different (HR 1.2, p=0.5). While PET+ status had a significant negative impact on PFS in both the CR/CRu (HR 2.6, p=0.015) and PR (HR 4.3 p=0.018) patient groups, there was no difference in outcome between CR/CRu vs. PR patients within the PET+ (HR 1.5 p=0.42) and PET- (HR 1.0 p=0.98) subgroups.
When only patients randomised for the maintenance element of the PRIMA study were considered, post-treatment PET+ (15/59) remained predictive of 3yr PFS (27 vs. 69%, HR 3.1, p=0.005) in the observation arm, but post-treatment PET+ (9/47) was not significantly associated with an adverse outcome in patients receiving rituximab maintenance (3-year PFS 56 vs. 81%, HR 2.2, p= 0.18).
In a multivariate Cox model including responding patients the following factors were negative predictors of PFS: post-treatment PET+ (HR 3.1 p<0.0014); R-CVP induction therapy (HR 2.8, p<0.014); and baseline β2M ≥3 (HR 2.6 p<0.0042), while conventional PR and FLIPI were not.
This PRIMA sub-study demonstrates that post-treatment PET-CT is a powerful predictor of PFS that complements conventional response evaluation after first line immunochemotherapy for FL. Patients who are PET- can expect a prolonged PFS whether in conventional CR or PR, but for those remaining PET+, with a median 19 month PFS, the disease cannot be characterized as indolent. Future clinical trials should evaluate an FDG PET-CT response adapted approach focused on improving outcomes for this group.
Seymour:Roche: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Shpilberg:Roche: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal