Abstract
Abstract 854
Residual abnormalities of uncertain significance are frequently seen on post-therapy CT scans in patients (pts) with advanced-stage diffuse large B-cell lymphoma (DLBCL) following treatment with R-CHOP. However, the value of consolidative radiation therapy (XRT) to these sites is unknown. FDG-PET scanning may allow for the discriminate use of XRT to eradicate sites of residual disease.
Since 2005, pts with advanced-stage DLBCL in British Columbia (BC) have been treated with a systematic policy recommending a post-chemotherapy PET scan for pts with residual abnormalities ≥2cm on CT scan, followed by XRT to PET-positive sites that are amenable to radiation. Pts with a negative PET scan are observed (regardless of initial or residual bulk), while pts with a PET scan that is widely positive and not suitable for XRT are treated at the discretion of individual physicians. All PET scans are performed in a central location using a combined PET/CT scanner; staging PET scans are not routinely performed. Using the databases of the BC Cancer Agency Centre for Lymphoid Cancer and Department of Functional Imaging, we identified all pts with newly diagnosed advanced-stage DLBCL between January 2005 and June 2009 treated with R-CHOP who underwent a post-treatment PET scan based on this management algorithm. This analysis does not include pts with primary progressive disease; pts with a complete remission on post-treatment CT scan; pts who were HIV positive; or those with transformed lymphoma.
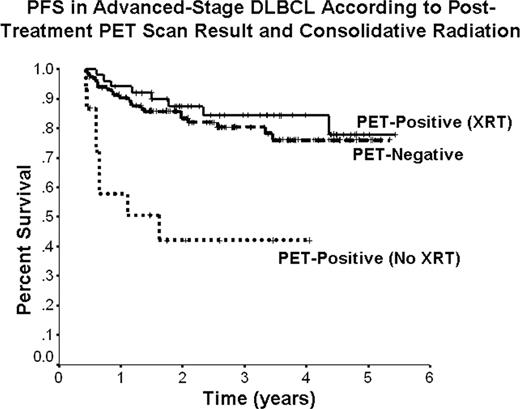
196 pts were identified with the following baseline characteristics: median age 64 y (range 18–89 y); 61% male; 62% stage III/IV; 41% PS>1; 21% >1 extranodal site; 57% elevated LDH; 46% bulky site ≥10cm; 56% IPI 0–2, 44% IPI 3–5. All pts received 3-weekly R-CHOP (6-8 cycles) with curative intent. Median follow-up for living pts is 32 mos (range 5–65 mos). 121/196 (62%) had a negative post-therapy PET (PET-Neg), 66/196 (34%) had a positive PET (PET-Pos), and 9 (4%) were indeterminate. Median SUV of PET-Pos scans was 3.4 (range 1.8–25). None of the PET-Neg pts received XRT. 51/66 (77%) of PET-Pos pts received XRT (3000-4000 cGy) to sites of PET positivity (46 single field, 5 multiple fields), with only 7 relapses to date. 15/66 (23%) PET-Pos pts did not receive XRT due to: multiple sites not amenable to XRT 11; physician choice 3; biopsy negative 1. Only 3/9 pts (33%) with an indeterminate PET received XRT. There was no difference in the 3-y PFS (80% v 75%, p=0.41) and 3-y OS (84% v 77%, p=0.10) between the PET-Neg and PET-Pos pts, respectively. The 3-y PFS was similar for PET-Pos pts who received XRT (84%) and PET-Neg pts (80%) and was superior to PET-Pos pts who did not receive XRT (42%). Pts with an indeterminate scan had a favorable outcome with a 3-y PFS of 89%.
Pts with advanced-stage DLBCL who have residual abnormalities on CT scan following R-CHOP and receive consolidative radiation to sites of PET positivity have an outcome similar to pts with a negative post-therapy PET. The favorable outcome observed in the PET-positive cohort treated with XRT is higher than expected from historical reports, suggesting a benefit for the rational use of PET-guided XRT following chemotherapy for DLBCL. Pts who have residual abnormalities on CT scan that are PET-negative should be spared indiscriminate exposure to radiation as the majority have been cured with systemic therapy.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal