Abstract
Abstract 4667
Current concepts of the pathophysiology of primary immune thrombocytopenia (ITP) reflect a complex interplay between antiplatelet antibodies, cytotoxic T-lymphocytes (CTL), T regulatory cells, and impaired bone marrow megakaryopoiesis. The mechanisms of ITP in the presence of monoclonal gammopathy of unknown significance (MGUS), a form of secondary ITP, are less well understood, yet treatment has been essentially the same as for primary ITP. Inhibition of antiplatelet CTL responses through apoptosis induction in clonal antiplatelet-antibody producing plasma cells and proteasome inhibition in CTLs may be achieved with bortezomib. However, bortezomib may cause transient isolated thrombocytopenia via presumed inhibition of marrow thrombopoiesis or enhanced platelet clearance peripherally.
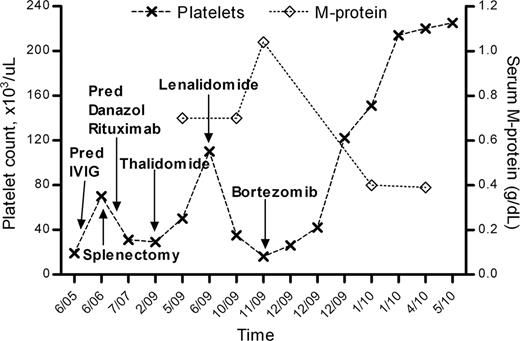
We used bortezomib in a 55 year-old female with IgG lambda monoclonal gammopathy and ITP refractory to previous treatment with corticosteroids, intravenous immunoglobulin, splenectomy, danazole, and rituximab, none of which induced a durable increase in her platelet counts to hemostatic concentrations. She suffered from repeated episodes of prolonged epistaxis, and when the platelet count fell below 10K/mm3, she experienced a life-threatening gastrointestinal hemorrhage. Otherwise, she had no anemia, her creatinine and calcium remained normal throughout, and skeletal surveys showed no evidence for myeloma. Repeated bone marrow examinations, reviewed at our institution, demonstrated lambda monotypic plasma cells always below 10%, and a normal female karyotype on metaphase cytogenetics. Her thrombocytopenia and bleeding episodes improved transiently on dexamethasone/IMiD combinations (thalidomide followed by lenalidomide), with concurrent reduction in total IgG by almost 50% (M-spike was not measured prior to IMiDs), however she became intolerant to thalidomide due to peripheral neuropathy and experienced diarrhea on lenalidomide. Her platelets decreased and her epistaxis worsened as her m-spike increased on dexamethasone single agent. We thus focused our treatment approach on more robust suppression of the monoclonal protein and initiated a course of weekly bortezomib (1.3 mg/m2), with dexamethasone (20 mg) on the day of and the day after bortezomib. After one month of therapy, the platelet count normalized, and she had no further bleeding episodes. The bortezomib dose was reduced to 1 mg/m2 and dexamethasone reduced to 20 mg weekly after 2 months, with persistently normal platelet counts thereafter. Her ITP resolution on bortezomib was accompanied by a decrease of her serum M-protein from 1.04 to 0.39 g/dL.
This case illustrates that bortezomib can be remarkably effective in refractory ITP with concurrent monoclonal gammopathy. Assuming similar pathophysiology, it might also have efficacy in primary refractory ITP. This case also raises the question of whether refractory ITP in the presence of a clonal plasma cell disorder should be considered as a myeloma defining symptom.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal