Abstract
Abstract 415
The ability to cure patients (pts) with advanced Hodgkin's Lymphoma (HL) with combination chemotherapy (CC) (MOPP and variants, ABVD and variants) represented a major milestone in oncology research, and CC became a paradigm for other malignancies. Further, the rationale for combined modality therapy (CMT) (radiation (RT) and CC) in HL evolved based on the high frequency of relapse in initially involved sites. As response rates and survival improved, newer treatments such as the combined modality Stanford V regimen were developed to shorten the duration of chemotherapy, add RT to sites of disease and reduce toxicity while maintaining or improving the cure rate. Indeed, the Stanford V regimen was tested and validated in a Phase II co-operative group trial (E1492) (J Clin Oncol 2000; 18:972). In order to investigate this approach against “standard” therapy, we conducted a randomized Phase III Intergroup trial of ABVD vs. the Stanford V regimen for patients with locally extensive or advanced HL.
The trial was designed to detect a 33% reduction in the failure free survival (FFS) hazard rate with Stanford V compared with ABVD, which corresponds to a difference in five-year FFS of 64% vs. 74%.
Patients with locally extensive (defined as clinical Ann Arbor Stage I-IIA/B and bulky mediastinal disease (BMD) (mass > 1/3 maximum intrathoracic diameter on standing postero-anterior chest x-ray or >/−10 cm on computerized tomography) or advanced (Ann Arbor Stage III or IV) HL were randomized to receive either ABVD × 6–8 cycles (C) (51% had 6 C, 35% had 8 C, 14% had <6 C) + 36 Gy (only in pts with BMD) or Stanford V × 12 weeks (95% had 12 weeks) + 36 Gy (for sites >5cm or for macroscopic splenic disease). The log-rank test was used to compare FFS for all eligible patients stratified on extent of disease (locally extensive vs. advanced), and number of International Prognostic Factor Project (IPFP) risk factors (0–2 vs. 3–7). An extended Cox model was also used to address non-proportional hazard between the two arms.
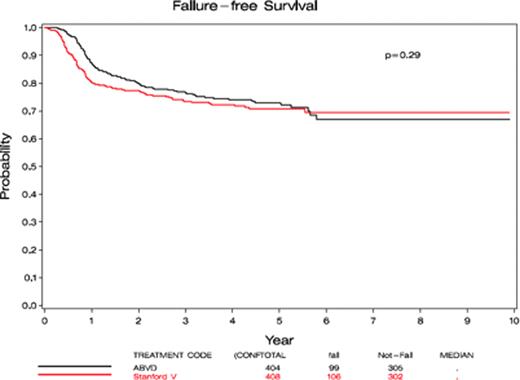
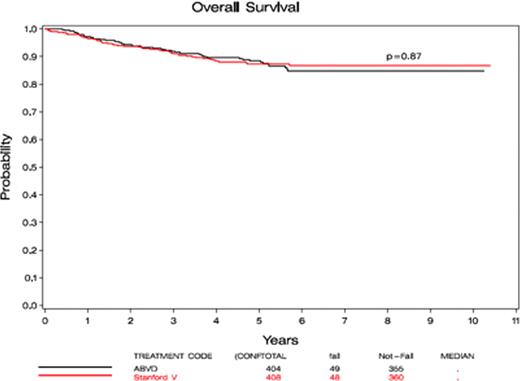
854 pts enrolled from April, 1999 to June, 2006 and 812 were eligible for analysis. 404 pts were randomized to ABVD and 408 to Stanford V. Median age was 33 yrs in both arms (range 16–83). 53% were men and 47% women; 4% had Stage I, 31% had Stage II, 39% had Stage III and 25% had Stage IV disease by Ann Arbor criteria. 35% of pts on ABVD and 35% on Stanford V had BMD. Three % of pts had nodular lymphocyte predominant HL, 77% of pts had nodular sclerosis HL, 14% had mixed cell HL. Age, stage, pathology and risk factors (0–2 vs. 3–7) were similar in both arms. In total, 65% were IPFP score 0–2 and 33% were 3–6. Response rate. There was no difference in response rates (RR) between the two arms (ABVD=72% CR+ CCR, 7.7% PR, 7.9% SD; Stanford V= 69 % CR +CCR, 7% PR and 10 % SD. 8% were not evaluable for response on ABVD and 9% on Stanford V. Toxicity was similar in both groups. The most frequent Grade 3 + 4 toxicity was neutropenia, and was similar between the 2 groups (76% Grade 3 + 4 in ABVD and 70% Grade 3+ 4 in Stanford V). Grade 5 toxicity was <1% in both groups. There was, however, more Grade 3 lymphopenia in Stanford V (78% vs. 42%, p< 0.0001) and more Grade 3 +4 sensory neuropathy in Stanford V (10%) than in ABVD (3%) (p< 0.0001). A total of 26 second primary cancers developed, 12 after ABVD and 14 after Stanford V (p=NS). FFS and OS. For 812 eligible patients, with a median follow up of 5.25 years, 5-year FFS was 73% for ABVD and 71% for Stanford V (p=0.29 by log rank) (Figure left); 5-year OS was 88% for ABVD and 87% for Stanford V (p=0.87 by log-rank, HR=0.97, 95% CI: 0.65 to 1.44) (Figure right) indicating no significant difference in either FFS or OS between the 2 arms.
In the largest Phase III intergroup trial of HL in North America, there was no significant difference in RR, FFS, OS, and 5-year toxicity when ABVD (+ RT for BMD) is compared with Stanford V (+RT for nodal sites >5 cm and macroscopic splenic disease). There was more Grade 3 lymphopenia (p< 0.0001) and more Grade 3 + 4 sensory neuropathy (p< 0.0001) on Stanford V. Thus ABVD (plus RT for BMD) remains the standard of care because Stanford V did not meet the objective of 33% improvement in FFS. For some patients, Stanford V, when given as described with RT, remains an acceptable alternative.
Friedberg:Genentech: Honoraria. Blum:Seattle Genetics: Research Funding; Novartis: Research Funding; Celgene: Research Funding. Horning:Genentech: Employment.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal