Abstract
Abstract 4104
The International Prognostic Scoring System (IPSS) for primary myelofibrosis (PMF) uses five predictors of inferior survival: age > 65 years, hemoglobin < 10 g/dL, leukocytes > 25 × 109/L, circulating blasts ≥ 1% and constitutional symptoms (Cervantes F et al. Blood 2009; 113: 2895). The dynamic IPSS (DIPSS) utilizes the same prognostic variables but can be applied at any time during the disease course (Passamonti F et al. Blood 2010; 115: 1703). IPSS-independent risk factors for survival have since been described and include unfavorable karyotype, red cell transfusion need and platelets < 100 × 109/L.
i) To determine if the aforementioned IPSS-independent risk factors for survival in PMF (i.e. unfavorable karyotype, red cell transfusion need and platelets < 100 × 109/L) are also DIPSS-independent.
ii) To develop and validate a refined DIPSS model that incorporates DIPSS-independent prognostic factors for survival.
iii) To establish a prognostic model for leukemia-free survival in PMF.
The Mayo Clinic database for PMF was used to identify patients in whom bone marrow histologic and cytogenetic information was obtained at the time of their referral. WHO criteria were used for PMF diagnosis and leukemic transformation (Vardiman JW et al. Blood 2009; 114: 937). None of the patients in the current study were included in the original group of patients used to describe DIPSS (Passamonti F et al. Blood 2010; 115: 1703).
A total of 793 patients met the above-stipulated criteria. The study population was divided into two groups based on whether or not patients were seen at the Mayo Clinic within (n=428; training set) or beyond (n=365; test set) their first year of diagnosis.
Multivariable analysis that included DIPSS risk category (low, intermediate-1, intermediate-2 and high risk), karyotype (favorable or unfavorable), platelet count (≥ or <100 × 109/L) and transfusion status (independent or dependent) was performed using the training set and all four variables were found to be significant as independent predictors of survival (p<0.0001, <0.0001, 0.0008 and 0.01, respectively).
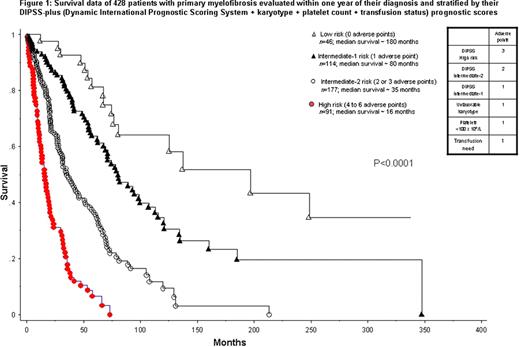
Using the respective hazard ratios (HR) obtained during the multivariable prognostic analysis in the training set, HR-weighted adverse points were assigned: 3 points for high-risk DIPSS, 2 points for intermediate-2 risk DIPSS, and 1 point each for intermediate-1 risk DIPSS, unfavorable karyotype, platelets < 100 × 109/L or transfusion need. Accordingly, a refined DIPSS model (i.e. DIPSS-plus) was devised using the training set (Figure 1) and subsequently validated in the test set (Figure 2): low-risk (0 adverse points), intermediate-1 risk (1 adverse point), intermediate-2 risk (2-3 adverse points) and high-risk (4-6 adverse points). Considering the entire group of 793 study patients, the respective median survivals were 185, 78, 35 and 16 months (p<0.0001).
Multivariable analysis identified platelet count (p=0.0007) and karyotype (p=0.04) but not DIPSS or transfusion status as independent predictors of leukemia-free survival. We used these two variables to classify patients into a low (favorable karyotype and platelets ≥ 100 × 109/L) or high (unfavorable karyotype or platelets < 100 × 109/L) risk category for leukemic transformation; the respective 5- and 10-year risk of leukemic transformation were 6% and 12% vs. 18% and 31%, respectively (p<0.0001; HR 3.3, 95% CI 1.9–5.6).
DIPSS-plus effectively incorporates prognostic information from karyotype, platelet count and transfusion status into the DIPSS prognostic model for PMF. Unfavorable karyotype or platelets <100 × 109/L is associated with a significantly higher risk of leukemic transformation in PMF.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal