Abstract
Abstract 3719
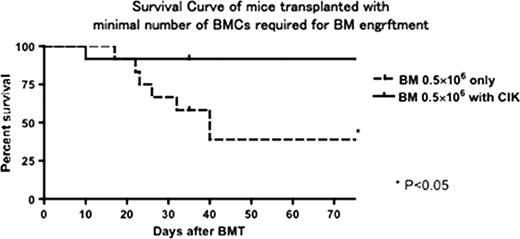
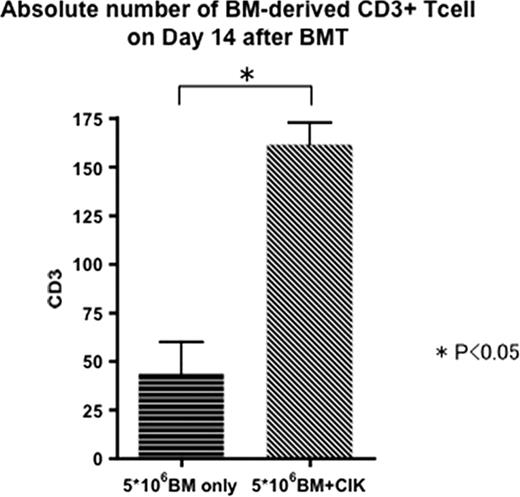
Cytokine-induced killer (CIK) cells are ex vivo–expanded T lymphocytes expressing both natural killer (NK)– and T-cell markers. We have reported that adoptive transfer of allogeneic CIK cells in a murine model caused minimal graft versus host disease (GVHD) with retention of antitumor activity mediated by NKG2D, which is an activating receptor expressed on NK cells. With the purpose of potential application of CIK cells in a clinical hematopoietic stem cell transplantation, the problem we have to consider next is whether CIK cells could promote an engraftment and facilitate an immune reconstitution. To this end, lethally irradiated BALB/c mice were injected with minimal number of MHC incompatible C57BL/6 bone marrow (BM) cells alone, in which almost half of mice died because of graft failure, or with CIK concurrently. The mice receiving BM plus CIK cells survived with 93% without GVHD, demonstrating that CIK cells significantly promote an engraftment (P<0.05). In particular, recovery of CD3+ T-cells was significantly faster (p<0.05) in the mice receiving BM plus CIK cells than those receiving BM cells alone. Next we further evaluated whether CIK cells also promote an engraftment in the mice receiving non-myeloablative conditioning using low dose total body irradiation. As expected, CIK cells promoted an engraftment and favored immunoreconstitution, especially from the early time point after BMT. In conclusion, our study clearly demonstrated that CIK cells promote an engraftment and facilitate an immure reconstitution without GVHD. As recent studies demonstrated that sufficient number of CIK cells could be expanded even from washouts of cord blood units bags, infusion of CIK cells would be a potent strategy for preventing a graft-failure in clinical settings, especially after cord blood transplantation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal