Abstract
Abstract 3450
Allogeneic hematopoietic cell transplantation (HCT) following a variety of reduced-intensity conditioning regimens has been reported to produce encouraging results in patients with AML. In these studies disease relapse was the main cause of treatment failure, with 2–4 year relapse rates ranging between 32–61% resulting in overall survivals of 28–45% at 2–4 years. Our goal here was to examine whether pre-HCT variables could identify patients at high risk for relapse following nonmyeloablative allogeneic HCT, who thus would become candidates for additional interventions to reduce the risk of AML relapse.
The data were derived from 274 consecutive Seattle Consortium patients (median age: 60 years) with de novo or secondary AML who underwent allogeneic HCT from related or unrelated donors after conditioning with 2 Gy total body irradiation (TBI) with or without fludarabine (90 mg/m2) as recently reported (Gyurkocza et al., JCO 2010 Jun 10;28(17):2859–2867). Cox regression was used to perform multivariate analysis of risk factors for relapse in a subset of 231 patients in morphologic leukemia-free state (defined as less than 5% marrow blasts) with (n=134) or without (n=97) peripheral blood cell count recovery (defined as platelets > 100,000/ml and neutrophils > 1,000/ml) at the time of HCT. In this multivariate model, AML beyond 1st complete remission (CR1), unfavorable cytogenetics (according to SWOG criteria), incomplete peripheral blood cell count recovery before HCT, and shorter time between diagnosis and HCT were associated with statistically significantly higher risk of relapse (Table 1). From this multivariate model we developed a relapse risk score that summarizes the contribution of multiple risk factors by assigning weights based on the relative magnitude of the log hazard ratios associated with the principal risk factors. From a starting score of 0, points were added or subtracted based on the following factors: 2nd CR: +1 point; 3rd or later CR: +2 points; unfavorable cytogenetics: +1 point; absence of pre-HCT peripheral blood cell count recovery: +0.5 points; time from diagnosis to HCT > 18 months, -2 points (Table 2). Patients were then stratified into 2 relapse risk groups according to whether the total risk score was ≤0 (low-risk) or >0 (high-risk).
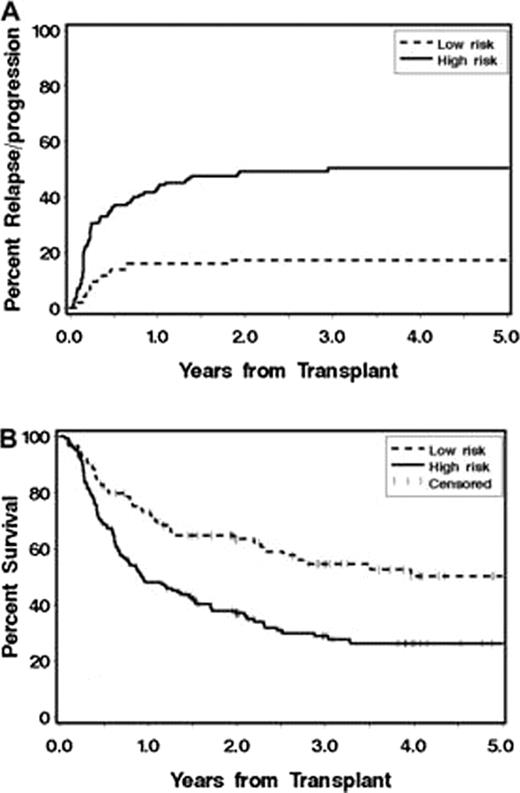
Stratification of patients according to the proposed Relapse Risk Score resulted in a clear separation of the two risk groups, with 5-year relapse rates of 50% and 17% in the high- and low-risk groups, respectively (Figure 1A). Five-year overall survival rates were 26% and 50% in the high- and low-risk groups, respectively (Figure 1B).
Our Relapse Risk Score may be a useful tool to identify patients with AML at high risk for relapse, who could potentially benefit from additional interventions to reduce the risk of relapse following allogeneic HCT. We are currently attempting validation in an independent cohort of patients with AML to make this Risk Score more generalizable.
Relapse/Progression (A) and Overall Survival (B) rates stratified by Relapse Risk Score.
Off Label Use: Off label usage of fludarabine, cyclosporine, tacrolimus and mycophenolate mofetil is discussed.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal