Abstract
Abstract 3085
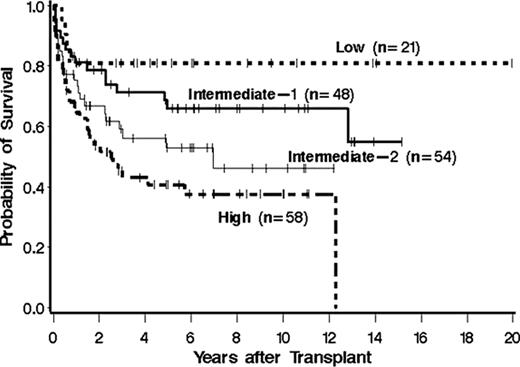
The International Working Group (IWG) has determined that prognosis in myelofibrosis is predicted by a scoring system that includes the following parameters: age > 65 years, constitutional symptoms, hemoglobin < 10 g/dL, leukocyte count > 25 × 109/L and circulating peripheral blasts ≥ 1%. Based on these factors patients may be placed into 4 separate categories: low, intermediate-1, intermediate-2 or high risk. The median survivals of these 4 groups are 135, 95, 48 and 27 months, respectively. The IWG scoring system has been validated in a dynamic prognostic model. However, there have been no publications evaluating the use of the IWG prognostic model in patients with myelofibrosis who receive hematopoietic cell transplantation (HCT).
We performed a retrospective review of 181 patients with a diagnosis of myelofibrosis who underwent HCT at the Fred Hutchinson Cancer Research Center between March, 1990 and November 2009. Twelve patients received an autologous transplant and 169 patients underwent an allogeneic transplant using an HLA-matched related (78), syngeneic (3), HLA-mismatched related (4), HLA-matched unrelated (66) or HLA-mismatched unrelated (18) donor. The median age at time of HCT was 51 (range: 12–78) years. Among the 169 patients who received allogeneic transplants, conditioning regimens consisted of oral busulfan, 16 mg/kg (136); oral busulfan, 7 mg/kg with TBI 12 Gy (9); TBI 12–13 Gy (4); Melphalan, 140 mg/kg (3); Fludarabine, 90 mg/m2 with TBI 2–4 Gy (16); and Treosulfan, 42 gm/m2 with Fludarabine, 150 mg/m2 (1). GVHD prophylaxis consisted of cyclosporin/methotrexate (99), tacrolimus/methotrexate (49), cyclosporin/mycophenolate (14) or tacrolimus/mycophenolate (4).
We were able to obtain the full set of parameters involved in calculating the IWG score in all 181 patients. Historical records pre-transplant and arrival records prior to transplant were reviewed. Patients were assigned to the highest possible IWG score based on age at time of HCT, history of constitutional symptoms, hemoglobin < 10 g/dL or transfusion dependence at time of transplant, history of leukocyte counts > 25 × 109/L, and history of peripheral blasts ≥ 1%. Based upon these parameters, there were 21 patients with low risk, 48 patients with intermediate-1, 54 patients with intermediate-2, and 58 patients with high risk disease. The IWG score was highly predictive of survival in the post-transplant setting with a hazard ratio (HR) of 4.4 (95% CI 1.6–12.5, p=0.005) for mortality in high risk patients compared to low risk patients. Patients in the low risk category had a significantly lower risk of relapse HR=0 (95% CI 0, p=0.046) in comparison to patients with high risk disease. In addition, patients with high risk disease had a significantly greater risk of transplant related mortality HR=3.7 (95% CI 1.3–11, p=0.016) in comparison to patients with low risk disease. This is the first examination of post-transplant outcomes by the pre-transplant IWG score. This analysis suggests that patient and disease characteristics considered in the IWG score and shown to be of prognostic significance at diagnosis also predict post-transplant survival. These findings, with a follow-up extending to two decades, indicate that while transplantation was curative for a proportion of patients, it could not completely overcome the risk conveyed by pre-transplant risk factors. It is our hope that future studies will use this information to address the optimal timing of appropriate interventions including HCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal