Abstract
Abstract 211
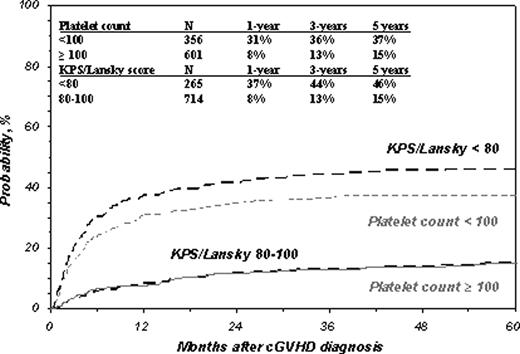
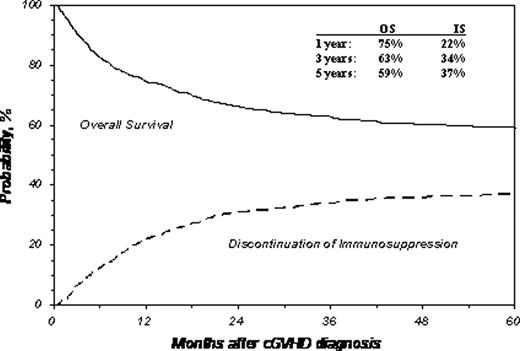
The adverse impact of chronic GVHD (cGvHD) on health and quality of life is especially critical in children because of their longer life expectancy and problems impacting growth and development. Although risk-factors for developing cGvHD in children are reported, little is known about risk factors for non-relapse mortality (NRM) in children with cGvHD. Identification of predictors for mortality in children with cGvHD could permit risk-adapted therapy, help plan for clinical trials and assist in counseling. We performed a multivariate analysis using data from CIBMTR to identify transplant- and cGvHD-related risk factors for NRM and survival in a cohort of 1117 subjects aged 0–20 years, transplanted from related donors, unrelated donors (URD), or unrelated cord blood (UCB) in 1995–2004 for acute myelogenous leukemia (AML), acute lymphoid leukemia (ALL), chronic myelogenous leukemia (CML) or myelodysplastic syndrome (MDS). Median age was 12 years. Characteristics of cGvHD at diagnosis were: progressive onset (49%), total bilirubin >2 mg/dL (16%), thrombocytopenia (platelets <100 × 109/L, 32%) and Karnofsky/Lansky (KPS/L) score <80 (24%). Probabilities of NRM at 1, 3, and 5 years after diagnosis of cGvHD were 17% (95% CI: 14–19%), 22% (20-25%) and 24% (21-27%), respectively. Multivariate analysis indentified four factors significantly associated (p<0.01) with higher NRM: (1) HLA-partially-matched or -mismatched URD; (2) peripheral blood cell graft; (3) KPS/L <80 at cGVHD diagnosis; and (4) platelets <100 × 109/L at cGVHD diagnosis. Survival after diagnosis of cGVHD at 1-, 3- and 5-years was 75% (72-77%), 63% (60-66%), and 59% (56-62%). Factors significantly associated with worse survival were: (1) age >10 years; (2) transplant from an HLA-partially-matched or -mismatched URD; (3) advanced disease at transplant; (4) KPS/L <80; and (5) platelets <100 × 109/L. The cumulative incidence of NRM at 5 years was higher for children with KPS/L <80 (46%; CI: 40–52%) than for those with a higher KPS/L score (15%; CI: 12–18%; p<0.001). This translated to poorer survival of 42% (36-48%) vs. 66% (CI: 63–70%; p<0.001), respectively. 5 year cumulative incidence of NRM was also higher in children with platelets <100 × 109/L: 37% (32-43%) vs. 15% (CI: 12–18%; p<0.001). This also resulted in poorer survival (47%, CI: 42–52%; vs. 67%, CI: 63–71%; p<0.001). Cumulative incidence of discontinuation of systemic immune suppression (death and relapse treated as competing risks) at 1, 3 and 5 years after diagnosis of cGvHD were 22% (20-25%), 34% (31-37%), and 37% (34-40%). In conclusion, we identified several factors adversely correlated with NRM and survival children with cGvHD. The correlation between peripheral blood cell grafts and increased NRM without poorer survival may be explained by fewer relapses. This is the first large study elucidating factors affecting outcome after diagnosis of cGvHD in children. Our results may be useful for risk stratification.
Close modalClose modal
| Survival . | NRM . | |||||||
|---|---|---|---|---|---|---|---|---|
| . | Relative Risk . | 95% CI . | P . | Relative Risk . | 95% CI . | P . | ||
| Age (baseline: 0–9 years) | ||||||||
| 10-19 | 1.32 | 1.09 | 1.60 | 0.005 | NS | |||
| KPS/L (baseline: 80–100) | <.001 | <.001 | ||||||
| <80 | 1.89 | 1.52 | 2.34 | <.001 | 3.01 | 2.29 | 3.96 | <.001 |
| unknown | 1.34 | 1.00 | 1.78 | 0.05 | 1.64 | 1.12 | 2.43 | 0.015 |
| Platelets (x10e9/L) (baseline: ≥ 100) | <.001 | <.001 | ||||||
| <100 | 1.63 | 1.32 | 2.01 | <0.001 | 2.32 | 1.76 | 3.07 | <.001 |
| Unknown | 1.33 | 0.99 | 1.78 | 0.06 | 1.73 | 1.18 | 2.52 | 0.005 |
| Donor (baseline: HLA-identical siblings) | 0.003 | <0.001 | ||||||
| Other related | 1.68 | 1.13 | 2.52 | 0.011 | 1.67 | 0.96 | 2.96 | 0.07 |
| HLA-well-matchedunrelated | 1.40 | 1.02 | 1.94 | 0.04 | 1.25 | 0.80 | 1.96 | 0.33 |
| Partially matched unrelated | 1.69 | 1.23 | 2.31 | 0.001 | 1.94 | 1.28 | 2.94 | 0.002 |
| Mismatched unrelated | 1.75 | 1.27 | 2.42 | <0.001 | 2.31 | 1.49 | 3.59 | <0.001 |
| No data | 1.02 | 0.64 | 1.62 | 0.94 | 1.22 | 0.60 | 2.13 | 0.71 |
| Disease State (baseline: Early) | <0.001 | 0.005 | ||||||
| Intermediate | 0.96 | 0.78 | 1.18 | 0.70 | 0.65 | 0.50 | 0.85 | 0.07 |
| Advanced | 1.56 | 1.19 | 2.04 | 0.001 | 0.92 | 0.63 | 1.35 | 0.68 |
| Graft (baseline: BM) | 0.002 | |||||||
| Blood | NS | 1.76 | 1.28 | 2.41 | <0.001 | |||
| Cord Blood | NS | 1.07 | 0.67 | 1.70 | 0.78 | |||
| Survival . | NRM . | |||||||
|---|---|---|---|---|---|---|---|---|
| . | Relative Risk . | 95% CI . | P . | Relative Risk . | 95% CI . | P . | ||
| Age (baseline: 0–9 years) | ||||||||
| 10-19 | 1.32 | 1.09 | 1.60 | 0.005 | NS | |||
| KPS/L (baseline: 80–100) | <.001 | <.001 | ||||||
| <80 | 1.89 | 1.52 | 2.34 | <.001 | 3.01 | 2.29 | 3.96 | <.001 |
| unknown | 1.34 | 1.00 | 1.78 | 0.05 | 1.64 | 1.12 | 2.43 | 0.015 |
| Platelets (x10e9/L) (baseline: ≥ 100) | <.001 | <.001 | ||||||
| <100 | 1.63 | 1.32 | 2.01 | <0.001 | 2.32 | 1.76 | 3.07 | <.001 |
| Unknown | 1.33 | 0.99 | 1.78 | 0.06 | 1.73 | 1.18 | 2.52 | 0.005 |
| Donor (baseline: HLA-identical siblings) | 0.003 | <0.001 | ||||||
| Other related | 1.68 | 1.13 | 2.52 | 0.011 | 1.67 | 0.96 | 2.96 | 0.07 |
| HLA-well-matchedunrelated | 1.40 | 1.02 | 1.94 | 0.04 | 1.25 | 0.80 | 1.96 | 0.33 |
| Partially matched unrelated | 1.69 | 1.23 | 2.31 | 0.001 | 1.94 | 1.28 | 2.94 | 0.002 |
| Mismatched unrelated | 1.75 | 1.27 | 2.42 | <0.001 | 2.31 | 1.49 | 3.59 | <0.001 |
| No data | 1.02 | 0.64 | 1.62 | 0.94 | 1.22 | 0.60 | 2.13 | 0.71 |
| Disease State (baseline: Early) | <0.001 | 0.005 | ||||||
| Intermediate | 0.96 | 0.78 | 1.18 | 0.70 | 0.65 | 0.50 | 0.85 | 0.07 |
| Advanced | 1.56 | 1.19 | 2.04 | 0.001 | 0.92 | 0.63 | 1.35 | 0.68 |
| Graft (baseline: BM) | 0.002 | |||||||
| Blood | NS | 1.76 | 1.28 | 2.41 | <0.001 | |||
| Cord Blood | NS | 1.07 | 0.67 | 1.70 | 0.78 | |||
NS=Not Significant
Cumulative Incidence of NRM by Platelets and KPS/L at Diagnosis of cGvHD
Cumulative Incidence of NRM by Platelets and KPS/L at Diagnosis of cGvHD
Survival and Cumulative Incidence of Discontinuation of Immune Suppression
Survival and Cumulative Incidence of Discontinuation of Immune Suppression
Disclosures:
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2010 by The American Society of Hematology
2010

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal