Abstract
MLL-rearranged acute lymphoblastic leukemia (ALL) represents an unfavorable type of leukemia that often is highly resistant to glucocorticoids such as prednisone and dexamethasone. Because response to prednisone largely determines clinical outcome of pediatric patients with ALL, overcoming resistance to this drug may be an important step toward improving prognosis. Here, we show how gene expression profiling identifies high-level MCL-1 expression to be associated with prednisolone resistance in MLL-rearranged infant ALL, as well as in more favorable types of childhood ALL. To validate this observation, we determined MCL-1 expression with quantitative reverse transcription–polymerase chain reaction in a cohort of MLL-rearranged infant ALL and pediatric noninfant ALL samples and confirmed that high-level MCL-1 expression is associated with prednisolone resistance in vitro. In addition, MCL-1 expression appeared to be significantly higher in MLL-rearranged infant patients who showed a poor response to prednisone in vivo compared with prednisone good responders. Finally, down-regulation of MCL-1 in prednisolone-resistant MLL-rearranged leukemia cells by RNA interference, to some extent, led to prednisolone sensitization. Collectively, our findings suggest a potential role for MCL-1 in glucocorticoid resistance in MLL-rearranged infant ALL, but at the same time strongly imply that high-level MCL-1 expression is not the sole mechanism providing resistance to these drugs.
Introduction
Acute lymphoblastic leukemia (ALL) in infants (ie, children < 1 year of age) is characterized by an exceptionally high incidence (∼ 80% of the cases) of chromosomal translocations affecting the MLL gene.1,2 These chromosomal abnormalities, believed to be initiating events in leukemogenesis, usually involve reciprocal translocations fusing the N-terminal portion of the MLL gene to the C-terminal region of one of its translocation partner genes, of which more than 50 have been described.3,4 The presence of MLL rearrangements represents the most important independent predictor of an adverse outcome.1,5 Although current therapies for pediatric ALL in general result in long-term survival in more than 80% of the cases, these therapies fail in more than 50% of infants diagnosed with MLL-rearranged ALL.1
A major obstacle hampering successful treatment results in MLL-rearranged infant ALL is cellular resistance to several drugs used in the treatment of ALL. In vitro studies showed that MLL-rearranged infant ALL cells are particularly highly resistant to prednisolone,6 the spearhead drug of ALL treatment regimes. Moreover, approximately 30% of the infant patients with MLL-rearranged ALL show a poor prednisone response in vivo, defined as the presence of at least 1000 leukemic blasts/μL after a 7-day window of prednisone monotherapy.1,7 In contrast, among children older than 1 year of age (noninfants) diagnosed with ALL, less than 10% of the patients show a poor in vivo response to prednisone.8 Both in vitro prednisolone sensitivity as well as the in vivo prednisone response are predictive for clinical outcome in pediatric ALL in general.7,9,10 Thus, the poor prognosis for MLL-rearranged ALL may to a large extent be associated with prednisone resistance. Therefore, overcoming resistance to this drug may be an important step toward a more favorable prognosis for MLL-rearranged leukemias.
Comparing gene expression profiles of pediatric patients with ALL (> 1 year of age) either in vitro sensitive or resistant to prednisolone, we recently found increased expression of the antiapoptotic BCL-2 family member MCL-1 in prednisolone-resistant patients samples.11 MCL-1 is considered an important cell survival factor in peripheral blood B lymphocytes12 and is often overexpressed in hematopoietic malignancies, including B cell chronic lymphoblastic leukemia (CLL) and multiple myeloma (MM).13,14 Here, we show that increased MCL-1 expression is not only associated with in vitro prednisolone resistance in pediatric ALL but also prominently in MLL-rearranged infant ALL. MCL-1 expression appears to be one of the few overlapping genes that commonly discriminates between prednisolone resistance and sensitivity when gene expression signatures associated with prednisolone resistance for both of these patient groups are compared. Furthermore, we demonstrate that among infant patients with MLL-rearranged ALL elevated MCL-1 expression is predictive for both the in vitro prednisolone as well as to some extent for the in vivo prednisone response. Finally, we demonstrate that reducing MCL-1 protein expression moderately sensitizes prednisolone-resistant MLL-rearranged leukemia cells to this drug in vitro.
Methods
Patient samples
Untreated primary bone marrow and/or peripheral blood samples from infants (< 1 year of age) diagnosed with ALL were collected at the Erasmus Medical Center (MC)–Sophia Children's Hospital and other hospitals participating in the INTERFANT-99 treatment study.1 Samples from pediatric patients older than 1 year (noninfants) with ALL were obtained from our cell bank at the Erasmus MC–Sophia Children's Hospital. Approval for these studies was obtained from the Erasmus MC Institutional Review Board. Informed consent was obtained according to the Declaration of Helsinki.
Within 24 hours after sampling, mononuclear cells were isolated by density gradient centrifugation with the use of Lymphoprep (density, 1.077 g/mL; Nycomed Pharma) and resuspended in RPMI 1640 medium (Dutch modification without l-glutamine; Invitrogen Life Technologies) supplemented with 20% fetal calf serum (Integro), 2mM l-glutamine (Invitrogen), 5 μg/mL insulin, 5 μg/mL transferrin, 5 ng/mL sodium selenite (ITS media supplement; Sigma-Aldrich), 100 IU/mL penicillin, 100 μg/mL streptomycin, 0.125 μg/mL Fungizone, and 0.2 mg/mL gentamycin (Invitrogen). Contaminating nonleukemic cells were removed with the use of immunomagnetic beads as described elsewhere.15 All samples used contained more than 90% leukemic cells, as determined morphologically on May-Grünwald-Giemsa (Merck)–stained cytospins.
As part of the INTERFANT-99 study, the infant ALL samples were screened for the presence of MLL rearrangements by fluorescence in situ hybridization analysis, and the type of translocation was determined with the use of polymerase chain reaction (PCR) analysis.1 An overview of available patient characteristics and clinical parameters are listed in supplemental Table 1 (available on the Blood website; see the Supplemental Materials link at the top of the online article).
In vitro prednisolone cytotoxicity and in vivo prednisone response
In vitro prednisolone (Bufa) cytotoxicity was determined using the methyl thiazole tetrazolium (MTT) assay as extensively described before.16 The in vivo response to prednisone in infant patients with ALL was determined after a 7-day window of prednisone monotherapy (before combination chemotherapy) as part of the INTERFANT-99 treatment protocol.1 Patients are defined as prednisone poor responders (PPRs) when at least 1000 leukemic blasts/μL peripheral blood remain present after the 7-day prednisone window. In cases when the amount of leukemic blasts drops below 1000/μL, the patients are defined as prednisone good responders (PGRs).
Microarray analysis of prednisone-sensitive and prednisone-resistant ALL samples
Patient samples were characterized as in vitro sensitive or resistant to prednisolone based on the LC50 value (ie, the concentration of prednisolone lethal to 50% of the leukemic cells), as obtained from MTT assays (described in “In vitro prednisolone cytotoxicity and in vivo prednisone response”). Samples were defined as prednisolone-sensitive at LC50 values less than 0.1 μg/mL prednisolone and prednisolone-resistant at LC50 values greater than 150 μg/mL prednisolone. Gene expression data (Affymetrix HU133A microarrays) were normalized using dChip17 and were filtered with a maximum−minimum = 100, and maximum/minimum = 4. The probe sets that correlated with sensitive/resistant distinction were determined using a signal-to-noise statistic and permutation testing. The accuracy of the gene expression signatures were assessed with a cross-validation approach as described previously.18 Briefly, for both the infant and noninfant ALL signatures separately, one sample was withheld, and the specified number of probe sets that best correlated with the prednisolone sensitive/resistant class distinction were identified. Next, the class of the withheld sample was determined on the basis of the gene expression pattern of the probe sets identified in this manner. This process was repeated for all samples, and the error rate in class prediction was determined and plotted against the number of probe sets used to build the model. The models were generated with 1 to 65 probe sets. The raw microarray data are listed in supplemental Table 2. All microarray data can be found in the GEO public database under accession no. GSE19143.19
Quantitative real-time PCR analysis
Total RNA was extracted from a minimum of 5 × 106 leukemic cells using TRIzol reagent (Invitrogen) according to the manufacturer's instructions, and quantified on a spectrophotometer. The integrity of the extracted RNA was assessed on 1% agarose gels. Extracted RNA was reverse transcribed, and the obtained cDNA was used to quantify MCL-1 mRNA expression relative to the endogenous housekeeping gene RNaseP, using quantitative real-time PCR (TaqMan) as described previously.20 Primer combinations used to amplify MCL-1 were as follows: forward, 5′-CGC CAA GGA CAC AAA G-3′, and reverse, 5′-AAG GCA CCA AAA GAA ATG-3′; for RNaseP the primers were forward, 5′-TTG GGA AGG TCT GAG ACT A-3′, and reverse, 5′-TCA GCC ATT GAA CTC ACT T-3′. The dual-labeled TaqMan probed used to detect amplified sequences were MCL-1, 5′-(FAM)-TTT CAG CGA CGG CGT AACA-(TAMRA)-3′, and for RNaseP, 5′-(FAM)-AGG TCA GAC TGG GCA GGA GAT-(TAMRA)-3′.
Cell line culture
Both SEMK2 and MV4-11 cells were maintained in RPMI 1640 with l-alanyl-l-glutamine (Invitrogen) supplemented with 10% fetal calf serum (Integro), 100 IU/mL penicillin, 100 μg/mL streptomycin, and 0.125 μg/mL Fungizone (Invitrogen) and grown as suspension cultures at 37°C in humidified air containing 5% CO2. The SEMK2 represents a B-lineage MLL-rearranged ALL cell line,21 and MV4-11 is an MLL-rearranged acute myeloid leukemia (AML) cell line. Both cell lines harbor MLL translocation t(4;11) and are highly resistant to prednisolone in vitro.
RNA interference
MCL-1 knock-down in the prednisone-resistant MLL-rearranged ALL and AML cell lines SEMK2 and MV4-11 were performed essentially as described before.22 Briefly, the RNA interference sequence for human MCL-1, GGACTGGCTAGTTAAACAAAG, as well as a validated nonsilencing control (RHS1707; Open Biosystems) were cloned into the pPRIME-SFFV-GFP lentiviral vector that enables the efficient expression of short hairpin RNAs in hematopoietic cells from the RNA Polymerase II promoter SFFV. The vector contains a GFP that allows for marking of lentiviral integration. Virus was produced by transient transfection of 293FT with a 3:1:4 mixture of psPAX-2, pMD2G-VSVG (kind gifts of Dr D. Trono, University of Geneva), and pPRIME-SFFV-GFP. After 24 hours medium was refreshed, and virus-containing medium was harvested 48 hours after transfection. On filtration through a 0.45-μm cellulose acetate filter, the virus stock was used to infect SEMK2 or MV4-11 cells. Infected cells were analyzed for MCL-1 expression by immunoblotting, and the in vitro prednisolone sensitivity was determined by 2-day MTT assays performed in triplicate. These procedures were then repeated to establish reproducibility among independent experiments.
Immunoblotting
Sodium dodecyl sulfate–polyacrylamide gel electrophoresis and immunoblotting were performed essentially as described earlier.22 Total cellular protein lysates were resolved on polyacrylamide gels and transferred to a nitrocellulose membrane (Amersham Biosciences). The membranes were probed with a rabbit anti–Mcl-1 polyclonal antibody. After incubating with respective secondary antibodies conjugated with horseradish peroxidase, MCL-1 was visualized with the use of an enchanced chemiluminescence kit (Amersham Biosciences).
Results
Microarray analysis of prednisone-sensitive and prednisone-resistant ALL samples
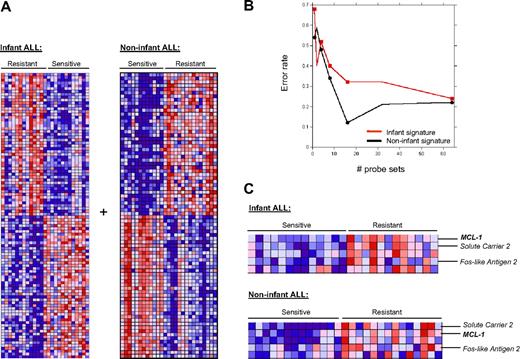
Comparing gene expression profiles between prednisolone-resistant and prednisolone-sensitive pediatric patients with ALL showed gene expression signatures associated with prednisolone resistance for both noninfant (> 1 year of age) or infant (< 1 year of age) ALL (Figure 1A). However, assessment of the accuracy of these signatures to predict prednisolone resistance or sensitivity with a cross-validation approach showed that, in particular in the infant ALL signature, the accuracy was rather low (Figure 1B). In other words, the error rate of reassigning infant ALL samples to their original class (ie, prednisolone sensitive or resistant) after being withheld from the analysis tended to be approximately 30% (Figure 1B), presumably because of the relatively low numbers of patient samples used to build these signatures. Therefore, we decided to merge both signatures in search for overlapping genes associated with prednisolone resistance in both patient groups. As shown in Figure 1C, elevated expression of Solute carrier 2 (SLC2), Fos-like antigen 2 (FOSL2), and MCL-1 appeared to be characteristic for both prednisolone-resistant infant as well as prednisolone-resistant noninfant ALL samples. Although both MCL-1 and SLC2 occurred in the top 50 up-regulated genes associated with prednisolone resistance in both the infant and noninfant ALL signatures (Figure 1A), this was not the case for FOSL2. Our approach to merge both signatures in search of genes that are associated with prednisolone resistance in both infant and noninfant ALL cases was not limited to the most significantly differentially expressed genes in both patient groups, but included the entire datasets. MCL-1, SLC2, and FOSL2 may therefore not be the most significantly up-regulated genes in either the infant or noninfant ALL signatures when evaluated separately, but they do represent the few genes associated with prednisolone resistance in both patient groups.
Gene expression profiling identifies high-level MCL-1 expression as a common marker for prednisone resistance among patients with childhood ALL. (A) The top 50 up-regulated probe sets correlate to either prednisone resistance or sensitivity in noninfant (> 1 year; n = 27) and infant (< 1 year; n = 25) patients with pediatric ALL. Raw microarray data can be found in supplemental Table 1. (B) Classification accuracy of prednisolone-sensitive or -resistant infant ALL or noninfant ALL samples on the basis of their gene expression profile. The error rate in class prediction is plotted against the number of probe sets used to build the model. (C) The overlapping genes associated with prednisone resistance in both the infant and noninfant ALL signatures. Merging the signatures shows that high-level MCL-1 expression is common to both noninfant and infant patients with ALL who are resistant to prednisone in vitro.
Gene expression profiling identifies high-level MCL-1 expression as a common marker for prednisone resistance among patients with childhood ALL. (A) The top 50 up-regulated probe sets correlate to either prednisone resistance or sensitivity in noninfant (> 1 year; n = 27) and infant (< 1 year; n = 25) patients with pediatric ALL. Raw microarray data can be found in supplemental Table 1. (B) Classification accuracy of prednisolone-sensitive or -resistant infant ALL or noninfant ALL samples on the basis of their gene expression profile. The error rate in class prediction is plotted against the number of probe sets used to build the model. (C) The overlapping genes associated with prednisone resistance in both the infant and noninfant ALL signatures. Merging the signatures shows that high-level MCL-1 expression is common to both noninfant and infant patients with ALL who are resistant to prednisone in vitro.
Correlation between high-level MCL-1 expression and in vitro resistance to prednisolone
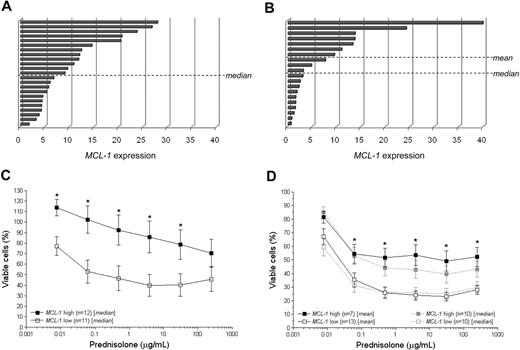
To validate our microarray data, we determined MCL-1 mRNA expression in MLL-rearranged infant ALL (n = 23) and noninfant ALL (n = 20) samples with the use of quantitative real-time PCR (TaqMan). For the sake of uniformity, infant ALL samples not carrying translocations of the MLL gene were intentionally excluded from these experiments, because the prognosis (and therapy response) of these patients are significantly more favorable compared with infant patients with MLL-rearranged ALL. Among both patient groups, we observed a wide and continuous range of MCL-1 expression levels (Figure 2A and 2C). With the use of the median or mean MCL-1 expression as a cutoff, we divided the samples into 2 groups either expressing “high” or “low” MCL-1 levels. For the infant patients with MLL-rearranged ALL the median expression coincided with the mean expression value. Next, we compared the in vitro prednisolone response between patients displaying high or low MCL-1 expression among both patient groups separately. As expected, MLL-rearranged infant ALL and pediatric noninfant ALL samples displaying high MCL-1 expression were significantly (P < .05) more resistant to prednisolone that were patients expressing lower levels of MCL-1 (Figure 2B,D). Interestingly, high level MCL-1 expression was also associated with the glucocorticoid dexamethasone (closely related to prednisolone), but not with increased resistance to unrelated drugs such as l-asparaginase, vincristine, daunorubicin, and cytarabine (supplemental Figure 1).
High-level MCL-1 expression is associated with in vitro prednisolone resistance in both MLL-rearranged infant ALL and noninfant pediatric precursor B-ALL. Distribution of the relative MCL-1 expression as determined by quantitative real-time RT-PCR (TaqMan) analyses among patients with (A) MLL-rearranged infant ALL and (B) noninfant (children > 1 year of age) B-ALL. Dotted lines either indicate the mean or median expression among both patient groups. Among the MLL-rearranged infant ALL cases, the median and mean MCL-1 expressions coincided. The median or mean MCL-1 expression level was used as the cutoff between patients, dividing the patients into groups displaying “high” or “low” MCL-1 expression. Mean cytotoxic dose-response curves for prednisolone in patients characterized by high or low MCL-1 expression are shown for patients with (C) MLL-rearranged infant ALL and (D) noninfant ALL, respectively. Differences in mean cytotoxicity responses between patient groups were statistically analyzed using the 2-tailed Student t test. Error bars represent SEM. *Indicates significant differences between the means of the groups at P < .05.
High-level MCL-1 expression is associated with in vitro prednisolone resistance in both MLL-rearranged infant ALL and noninfant pediatric precursor B-ALL. Distribution of the relative MCL-1 expression as determined by quantitative real-time RT-PCR (TaqMan) analyses among patients with (A) MLL-rearranged infant ALL and (B) noninfant (children > 1 year of age) B-ALL. Dotted lines either indicate the mean or median expression among both patient groups. Among the MLL-rearranged infant ALL cases, the median and mean MCL-1 expressions coincided. The median or mean MCL-1 expression level was used as the cutoff between patients, dividing the patients into groups displaying “high” or “low” MCL-1 expression. Mean cytotoxic dose-response curves for prednisolone in patients characterized by high or low MCL-1 expression are shown for patients with (C) MLL-rearranged infant ALL and (D) noninfant ALL, respectively. Differences in mean cytotoxicity responses between patient groups were statistically analyzed using the 2-tailed Student t test. Error bars represent SEM. *Indicates significant differences between the means of the groups at P < .05.
Correlation between high-level MCL-1 expression and in vivo prednisone resistance
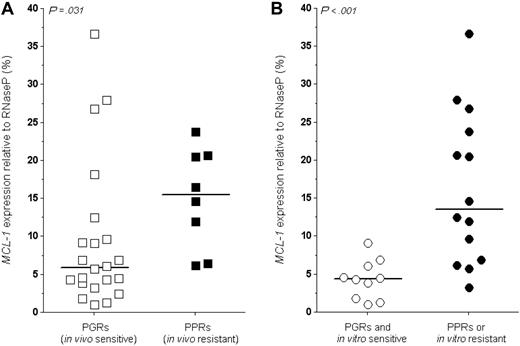
The 7-day window of prednisone monotherapy (before the combination chemotherapy) implemented in the INTERFANT-99 treatment protocol and used to ascribe infant patients with ALL to either the standard-risk (PGR) or high-risk (PPR) arm of the protocol provided an opportunity to correlate MCL-1 expression levels with the in vivo prednisone response in infant patients with MLL-rearranged ALL. This showed that the MCL-1 expression is significantly (P = .031) higher in infant patients with MLL-rearranged ALL with a PPR in vivo (Figure 3A). Of note is that the 3 patients with the highest MCL-1 expression appeared to have shown a good prednisone response in vivo (Figure 3A). However, despite their favorable in vivo prednisone response, these patients all relapsed, 2 of which within the first year of diagnosis. Nevertheless, a clear relationship between the level of MCL-1 expression and clinical outcome or risk of relapse was not found, possibly because of the low numbers of patient samples for which these data were available. Moreover, the correlation between the in vitro prednisolone and in vivo prednisone responses was definitely not absolute, because some patients showing a PPR in vivo appeared sensitive to prednisolone in vitro and vice versa. Figure 3B shows the differences in MCL-1 expression in infant patients with MLL-rearranged ALL who are sensitive to prednisone both in vitro and in vivo, compared with patients resistant to prednisone either in vitro or in vivo. This comparison underlines the obscure relationship between the prednisolone response in vitro and the prednisone response in vivo, but it also shows that the MCL-1 expression in infant patients with MLL-rearranged ALL who are sensitive to prednisolone in vitro and respond well to prednisone in vivo is markedly reduced compared with more resistant patients.
High-level MCL-1 expression is associated with in vivo prednisone resistance in MLL-rearranged infant ALL. (A) On the basis of a 7-day window of prednisone monotherapy, patients with MLL-rearranged infant ALL are classified as prednisone good responders (PGRs; < 1000 leukemic blasts/μL) or PPRs (≥ 1000 leukemic blasts/μL). The graph shows the relative MCL-1 expression as determined by quantitative real-time RT-PCR (TaqMan) in both patient groups. (B) The differences in relative MCL-1 expression in patients with infant ALL who are PGRs and are sensitive to prednisolone in vitro, compared with patients who are resistant either in vivo (PPRs) or in vitro. Dots represent individual patients; lines indicate the median MCL-1 expression level in each group. The difference between patient groups was statistically analyzed using the Mann-Whitney U test.
High-level MCL-1 expression is associated with in vivo prednisone resistance in MLL-rearranged infant ALL. (A) On the basis of a 7-day window of prednisone monotherapy, patients with MLL-rearranged infant ALL are classified as prednisone good responders (PGRs; < 1000 leukemic blasts/μL) or PPRs (≥ 1000 leukemic blasts/μL). The graph shows the relative MCL-1 expression as determined by quantitative real-time RT-PCR (TaqMan) in both patient groups. (B) The differences in relative MCL-1 expression in patients with infant ALL who are PGRs and are sensitive to prednisolone in vitro, compared with patients who are resistant either in vivo (PPRs) or in vitro. Dots represent individual patients; lines indicate the median MCL-1 expression level in each group. The difference between patient groups was statistically analyzed using the Mann-Whitney U test.
Down-regulation of MCL-1 induces sensitivity to prednisolone
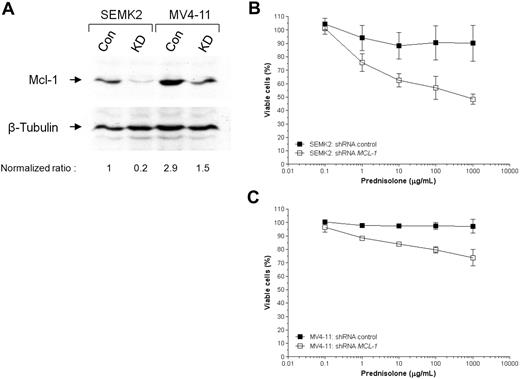
To determine whether MCL-1 protein down-regulation in prednisolone-resistant leukemia cells reverses the resistant phenotype and induces prednisolone sensitivity, we knocked-down MCL-1 expression in the MLL-rearranged ALL and AML cell lines SEMK2 and MV4-11 with the use of RNA interference. As shown in Figure 4A, the level of MCL-1 protein expression in SEMK2 cells was successfully decreased (but not completely diminished) by transfecting these cells with vectors encoding short hairpin RNAs against human MCL-1 by viral infection (Figure 4A). Compared with SEMK2, MV4-11 expressed an approximate 3-fold higher MCL-1 protein level, and the maximally achieved reduction in MCL-1 expression was approximately 50%. Control cells were either SEMK2 or MV4-11 cells virally infected with empty vectors only. Compared with the control cells, SEMK2 cells in which MCL-1 expression was reduced became more sensitive to prednisolone. MV4-11 cells, in which MCL-1 knock-down was less pronounced, only showed moderate sensitization to prednisolone (Figure 4C). In vitro prednisolone sensitivity was assessed by 2-day prednisolone cytotoxicity assay (MTT assay) performed in triplicate. Data shown in Figure 4B and C are MTT assay results derived from 2 independent RNA interference experiments.
Down-regulation of MCL-1 sensitizes prednisone-resistant MLL-rearranged ALL cells. (A) RNA interference experiments delivering short hairpin RNA(shRNA) molecules directed against human MCL-1 into prednisolone-resistant SEMK2 (MLL-rearranged ALL) or MV4-11 (MLL-rearranged AML) cells by viral infections, show severe suppression in MCL-1 protein expression compared with control cells (infected with empty vectors). The indicated ratios are normalized against β-tubulin and represent MCL-1 intensities relative to SEMK2 control cells (first lane) The effects of MCL-1 down-regulation on the in vitro prednisolone response on (B) SEMK2 or (C) MV4-11 cells were assessed by 2-day MTT cytotoxicity assays, performed in triplicate. The graphs show the mean prednisolone response curves in cells infected with either empty vectors (C indicates controls) or vectors encoding shRNAs against human MCL-1 (KD, knock-down), derived from 2 independent RNA interference experiments.
Down-regulation of MCL-1 sensitizes prednisone-resistant MLL-rearranged ALL cells. (A) RNA interference experiments delivering short hairpin RNA(shRNA) molecules directed against human MCL-1 into prednisolone-resistant SEMK2 (MLL-rearranged ALL) or MV4-11 (MLL-rearranged AML) cells by viral infections, show severe suppression in MCL-1 protein expression compared with control cells (infected with empty vectors). The indicated ratios are normalized against β-tubulin and represent MCL-1 intensities relative to SEMK2 control cells (first lane) The effects of MCL-1 down-regulation on the in vitro prednisolone response on (B) SEMK2 or (C) MV4-11 cells were assessed by 2-day MTT cytotoxicity assays, performed in triplicate. The graphs show the mean prednisolone response curves in cells infected with either empty vectors (C indicates controls) or vectors encoding shRNAs against human MCL-1 (KD, knock-down), derived from 2 independent RNA interference experiments.
Discussion
MLL-rearranged ALL represents an aggressive and difficult-to-treat type of leukemia commonly diagnosed in children younger than 1 year (ie, infants). Despite various attempts to intensify therapy to improve prognosis for these very young children, survival rates remain at best approximately 50%.1 Significantly contributing to this poor prognosis is cellular drug resistance. Leukemic cells from infant patients with MLL-rearranged ALL are highly resistant, both in vitro and in vivo, to glucocorticoids (such as prednisone and dexamethasone) which form the backbone of ALL treatment protocols. Because it has been established that both the in vitro prednisolone and in vivo prednisone response are highly predictive for clinical outcome among patients with ALL,7,9,10 overcoming glucocorticoid resistance may be an important step toward an improved outcome for MLL-rearranged ALL. For this, the biologic mechanism(s) that maintain resistance to these drugs should be elucidated and understood to be able to modulate glucocorticoid resistance.
Here, we show that high-level expression of the antiapoptotic BCL-2 family member MCL-1 is associated with in vitro prednisolone resistance in both MLL-rearranged infant ALL, as well as in noninfant pediatric ALL. The fact that high-level MCL-1 expression appeared to be associated with in vitro prednisolone resistance in both of these patient groups indicates that this may involve a general resistance mechanism protecting ALL cells from glucocorticoid-induced apoptosis. In subsequent experiments focusing on MLL-rearranged infant ALL samples, we confirmed that patients expressing high levels of MCL-1 not only are significantly more resistant in vitro to prednisolone but also to the closely related glucocorticoid dexamethasone (supplemental Figure 1). Furthermore, we demonstrate that, to some extent, high-level MCL-1 expression was associated with a poor response to prednisone in vivo. However, the range of MCL-1 expression in both the PGRs and the PPRs is pronounced, and the 3 patients expressing the highest levels of MCL-1 appeared to have experienced a good in vivo response to prednisone. This indicates that, despite the tendency of patients with a poor in vivo prednisone response expressing higher levels of MCL-1, the correlation is not entirely conclusive, suggesting that high-level MCL-1 expression may not be the sole mechanism driving prednisone resistance in vivo. In support of this, we did not find a convincing correlation between the level of MCL-1 expression and clinical outcome (for clinical parameters see supplemental Table 2). An alternative interpretation of this observation could be that modulation of prednisolone resistance alone may not be sufficient to significantly improve prognosis.
To validate the role of MCL-1 expression in maintaining prednisolone resistance in vitro, we conducted MCL-1 knock-down experiments, showing that prednisolone-resistant MLL-rearranged ALL (SEMK2) cells become more sensitive to this drug when MCL-1 protein expression is markedly reduced. In MLL-rearranged AML (MV4-11) cells, however, MCL-1 protein expression was markedly higher, and MCL-1 protein expression could only be reduced by approximately 50%. Consequently, the prednisolone-sensitizing effects in these cells were only moderate. Collectively, these results clearly show that merely reducing the levels of MCL-1 expression is not sufficient to completely reverse the prednisolone-resistant phenotype. Again, these observations emphasize that up-regulated MCL-1 expression presumably is not the only mechanism maintaining prednisolone resistance in MLL-rearranged infant ALL (see below).
As a member of the antiapoptotic BCL-2 protein family, MCL-1 may be expected to raise resistance to apoptosis induced by various chemotherapeutic drugs. However, we observed that elevated MCL-1 expression is only associated with resistance to the glucocorticoids prednisolone and dexamethasone, but not with resistance to other drugs used in the treatment of ALL such as vincristine, l-asparaginase, daunorubicin, and cytarabine (supplemental Figure 1). A possible explanation for this remarkable phenomenon may lie in both the mechanism by which MCL-1 exerts its antiapoptotic function and the way in which glucocorticoids induce apoptosis. Glucocorticoids specifically trigger apoptosis by inducing Ca2+ release from the endoplasmic reticulum and thereby increase the intracellular Ca2+ levels.23,24 These cytosolic Ca2+ signals are then transmitted to the mitochondria. Repetitive increases in mitochondrial Ca2+ levels eventually result in the release of cytochrome c, leading to apoptosis. MCL-1 is localized to the mitochondria and is able to inhibit mitochondrial Ca2+ signals, preventing cytochrome c release and apoptosis.25 Thus, increased MCL-1 expression in leukemic cells may result in resistance to glucocorticoids in ALL cells because of inhibition of the mitochondrial Ca2+ signals induced by these drugs. If so, the absent correlation between high-level MCL-1 expression and increased resistance to the other drugs tested would imply that apoptosis induced by these other drugs are less dependent on increasing cytosolic and mitochondrial Ca2+ levels. In support of this, we recently showed that in ALL cells vincristine and daunorubicin induced apoptosis do not require caspase-3 activation by the apoptosome (consisting of cytochrome c, Apaf-1 [apoptotic protease-activating factor-1], and pro-caspase 9),26,27 which can only be formed when cytochrome c is released from the mitochondria. Possibly, these agents initiate apoptosis in ALL cells using alternative mechanisms that are not affected by increased inhibition of mitochondrial Ca2+ signals established by elevated levels of MCL-1. However, suppression of mitochondrial Ca2+ signals most certainly is not the only mechanism by which MCL-1 may inhibit glucocorticoid-induced apoptosis. Erlacher et al28 demonstrated that the proapoptotic BH3-only proteins PUMA and BIM are required and rate limiting for glucocorticoid-induced apoptosis in lymphoid cells in vivo. In line with this, we recently showed that enforced overexpression of MCL-1 sequesters BIM in primary lymphocytes, preventing it from activating proapoptotic BAX/BAK, and thereby rendering resistance to glucocorticoid-induced apoptosis.29 Thus, the ability of MCL-1 to suppress mitochondrial Ca2+ signals and inhibit glucocorticoid-induced apoptosis not only depends on the MCL-1 expression level, but presumably is also influenced by the BIM and/or PUMA expression levels. Although our data did not identify significant up-regulated expression of BIM or PUMA to be a common feature among prednisolone-sensitive pediatric ALL samples, it remains possible that some patients express sufficient amounts of either BIM or PUMA to trigger glucocorticoid-induced apoptosis despite high MCL-1 expression. If so, this would further explain how some infant patients with MLL-rearranged ALL show a good in vivo response to prednisone, while at the same time displaying high-level MCL-1 expression.
We showed that down-regulation of MCL-1 expression in prednisolone-resistant MLL-rearranged ALL (SEMK2) cells to some extent induces prednisolone sensitivity. Although the prednisolone-sensitizing effects of MCL-1 down-regulation appeared moderate, the cytotoxic response tended to resemble that of prednisolone-sensitive MLL-rearranged infant ALL cells. Therefore, finding therapeutically applicable agents that are able to reduce MCL-1 expression in ALL cells during glucocorticoid treatment may increase the efficacy of these drugs and as such may contribute to the prevention of early relapse of the disease. Recently, we showed that rapamycin could represent such a glucocorticoid-sensitizing agent. Comparing the same gene expression signature of prednisolone resistance/sensitivity in noninfant patients with ALL as presented in Figure 1A with a database of drug-associated gene expression profiles (connectivity mapping) showed that rapamycin induces a gene signature that matches that of patients with prednisone-sensitive ALL.29 This study further showed that rapamycin could suppress MCL-1 expression, thereby sensitizing malignant lymphoid cells to glucocorticoids. Moreover, the glucocorticoid-sensitizing effects of rapamycin appeared to rely on activation of the AKT/mTOR pathway, and rapamycin is currently used in clinical trials for malignancies that depend on AKT/mTOR activation. Unfortunately, rapamycin did not result in MCL-1 down-regulation or to glucocorticoid sensitivity in primary MLL-rearranged infant ALL cells (M.L.D.B., unpublished data, 2008), suggesting that the AKT/mTOR pathway may not play a significant role in this type of leukemia. Nevertheless, our data emphasize that sustained high-level MCL-1 expression represents a general mechanism of glucocorticoid resistance among patients with ALL, including MLL-rearranged infant ALL cases. For this latter group of patients the challenge now is to identify compounds that do suppress MCL-1 expression in these cells. Several studies have reported compounds that induce apoptosis by targeting MCL-1. MCL-1 plays an important role in the survival of B-cell chronic CLL (B-CLL), as well as in MM cells, in which, like in MLL-rearranged ALL, abundant MCL-1 expression is also frequently observed.14,30 Recently, honokiol (a natural phenolic compound extracted from the root and stem bark of several species of Magnolia) was found to induce leukemic cell death in primary B-CLL cells by down-regulating MCL-1 expression.31 Similarly, 2 synthetic compounds, ie seliciclib (CYC202 or R-roscovitine) and R-etodolac (SDX-101), induced apoptosis in MM cells by directly targeting MCL-1.32,33 However, despite numerous attempts in our laboratory we observed that none of these compounds was able to reduce MCL-1 expression and to induce glucocorticoid sensitivity in MLL-rearranged ALL cells (R.W.S., unpublished data, 2008).
Taken together, our study shows an important role of MCL-1 in glucocorticoid resistance in MLL-rearranged infant ALL, warranting further studies to identify drugs that effectively down-regulate MCL-1 expression, to be coadministered during glucocorticoid-based treatment regimes. Our observations also strongly suggest that high-level MCL-1 expression presumably is not the sole mechanism maintaining glucocorticoid resistance, and additional studies in search for alternative or cooperating mechanisms remain important to fully understand and to eventually circumvent or overcome glucocorticoid resistance in patients.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank the members and participating hospitals of INTERFANT-99 for supporting this study by providing leukemic samples. Members of INTERFANT-99 are M. Campbell (Programa Infantil Nacional de Drogas Atineoplasicas), M. Felice (Argentina), A. Ferster (Children's Leukemia Group), I. Hann and A. Vora (UK Children's Cancer Study Group), L. Hovi (Nordic Society of Paediatric Haematology and Oncology), G. Janka-Schaub (Cooperative Study Group for Treatment of ALL), C. K. Li (Hong Kong), G. Mann (Berlin-Frankfurt-Munster Group-Austria), F. Mechinaud (French ALL Group), R. Pieters (Dutch Childhood Oncology Group), G. de Rossi and A. Biondi (Associazione Italiana Ematologia Oncologia Pediatrica), J. Rubnitz (St Jude Children's Research Hospital), M. Schrappe (Berlin-Frankfurt-Munster Group-Germany), L. Silverman (Dana-Farber Cancer Institute), J. Stary (Czech Paediatric Haematology), R. Suppiah (Australian and New Zealand Children's Haematology/Oncology Group), T. Szczepanski (Polish Paediatric Leukemia and Lymphoma Study Group), and M. Valscecchi and P. de Lorzenzo (Trial Operating Center).
This work was supported by the Sophia Foundation for Medical Research (SSWO grant 455), the Leukemia Research Fund (J.d.B.), and the Dutch Cancer Society (grant EMCR 2005-2662, R.W.S.).
Authorship
Contribution: R.W.S. designed and performed research and wrote the manuscript; M.L.D.B. and S.E.S. reviewed the manuscript; P.S., J.d.B., and J.H. performed research; M.G.V. and P.d.L. collected patient information and statistics; H.J.M.B. and S.A.A performed research and reviewed the manuscript; and R.P. designed the research and reviewed the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ronald W. Stam, Erasmus MC–Sophia Children's Hospital, Pediatric Oncology/Hematology, Rm Sp 2456, Dr Molewaterplein 60, PO Box 2060, 3000 CB Rotterdam, The Netherlands; e-mail: r.stam@erasmusmc.nl.