Consider a patient who presents with lymphadenopathy, splenomegaly, and pancytopenia and is discovered to have an atypical lymphocyte population with an acquired mutation in a gene crucial to cellular apoptosis. Conventional wisdom suggests this patient has cancer; however, if the somatic mutation is in FAS, then the diagnosis may be ALPS rather than malignancy.
In this issue of Blood, Dowdell and colleagues investigate the prevalence and clinical manifestations of somatic FAS-variant ALPS.1 Autoimmune lymphoproliferative syndrome (ALPS) is a disorder of abnormal lymphocyte survival caused by dysregulation of the Fas apoptotic pathway (see figure). Defective apoptosis leads to chronic lymphoproliferation (lymphadenopathy and hepatosplenomegaly), autoimmune disease (primarily autoimmune cytopenias), and a propensity to develop cancer. Until recently, diagnosis required meeting 3 criteria: (1) chronic nonmalignant lymphoproliferation; (2) elevated peripheral blood double-negative T cells (DNTs, cell phenotype: TCRα/β+, CD3+, CD4−, CD8−); and (3) defective in vitro Fas-mediated apoptosis, which requires culturing peripheral blood mononuclear cells (PBMCs) for at least 7 days, exposure to anti-Fas monoclonal antibody, and demonstration of a lack of apoptosis.
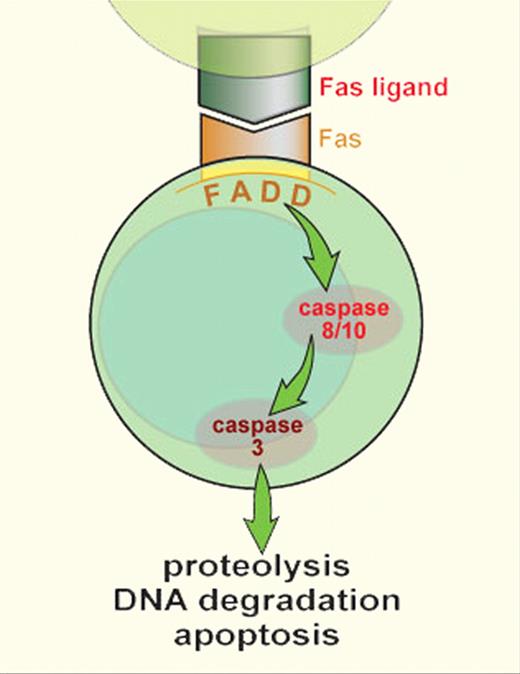
As part of the down-regulation of the immune response, activated T lymphocytes up-regulate Fas expression and activated B and T lymphocytes up-regulate expression of Fas-ligand. Fas and Fas-ligand interact through the Fas-activating death domain (FADD) to trigger the caspase cascade, leading to proteolysis, DNA degradation, and apoptosis. Germline mutations have been described in ALPS in FAS, Fas-ligand, and caspase 10. Somatic mutations have been identified only in FAS; however, they could be found in other genes with future study. Professional illustration by Sue Seif (used with permission).
As part of the down-regulation of the immune response, activated T lymphocytes up-regulate Fas expression and activated B and T lymphocytes up-regulate expression of Fas-ligand. Fas and Fas-ligand interact through the Fas-activating death domain (FADD) to trigger the caspase cascade, leading to proteolysis, DNA degradation, and apoptosis. Germline mutations have been described in ALPS in FAS, Fas-ligand, and caspase 10. Somatic mutations have been identified only in FAS; however, they could be found in other genes with future study. Professional illustration by Sue Seif (used with permission).
Seventy to 80 percent of ALPS patients have an identifiable genetic mutation. Most patients have germline mutations in FAS, and a smaller subset of patients have germline mutations in CASP10 and FASL. In 2004, Holzeva and colleagues made the seminal observation that ALPS can be caused by somatic mutations in FAS localized to the DNT compartment.2 DNTs do not survive in culture and the “gold standard” functional assay for ALPS assesses Fas signaling on “non-DNT” T lymphocytes. A small cohort of patients challenged the diagnostic algorithm with their normal in vitro Fas-mediated apoptosis.
Many issues about somatic FAS-variant ALPS are addressed in the article by Dowdell et al, including how prevalent this subtype is, how clinical manifestations compare with its germline counterpart, and whether there are biomarkers that identify these patients more easily than the current technique of sorting and enriching DNTs for FAS mutation analysis.
Dowdell et al studied a cohort of 31 patients with either ALPS-III or ALPS-phenotype. ALPS-III patients meet the current diagnostic triad and have no identifiable germline mutation. ALPS-phenotype patients have lymphoproliferation and elevated DNTs but normal in vitro Fas-mediated apoptosis. By sorting for DNTs, the authors identified FAS mutations in 12 patients. These mutations were found in less than 10% of PBMCs and not in buccal epithelial cells, suggesting they were somatic mutations. All mutations resulted in known or predicted functional loss of Fas signaling. These patients had clinical manifestations similar to their germline counterparts including lymph node size and incidence of autoimmune disease; however, they presented at an older age. The authors found that these patients were reliably identifiable by biomarkers that have been recently shown to predict germline FAS-ALPS, including markedly elevated IL-10, vitamin B12, sFasL, and IgG.3-5 These biomarkers are less robust in identifying other ALPS subtypes.
The high percentage of somatic FAS mutations in ALPS-phenotype patients is expected; however, the identification of somatic ALPS in type III patients is surprising. The published theory is that the Fas-mediated apoptosis assay is normal in somatic FAS-ALPS because DNTs do not survive in culture, and the functional defect is missed by performing the assay on nonmutated T-cell populations.2 Dowdell et al report abnormal apoptosis in the functional assay on unsorted PBMCs; however, they cannot identify a mutation on genetic analysis on the same PBMCs without DNT purification. This is an interesting but confounding finding that warrants further investigation and explanation. Many centers test for somatic mutations in the ALPS-phenotype patients but not routinely in type III patients. This report may lead to a paradigm shift.
These data suggest that somatic FAS mutations constitute the second largest group of known mutations in ALPS, affecting approximately 10% of patients. Accordingly, a large number of patients with clinical features of ALPS do not fulfill current diagnostic criteria. On the basis of the findings by Dowdell et al as well as recent papers highlighting the ability to use biomarkers to diagnose ALPS,3-5 an international ALPS consensus conference was held at the National Institutes of Health in 2009 with the goal of defining a better diagnostic algorithm. This new algorithm will be published shortly and incorporates genetic information, biomarkers, and histopathology in the diagnostic schema. This is an exciting time in ALPS research, as key insights into the diagnosis, pathophysiology, and treatment of ALPS have been recently published. New insights into signaling pathways, such as mTOR, that may be dysregulated in ALPS have been reported, leading to novel and effective treatments.6
ALPS may be a premalignant condition, as 10% to 20% of patients with germline FAS mutations develop cancer, most commonly lymphoma. This is consistent with the identification of somatic FAS mutations in both Hodgkin and non-Hodgkin lymphoma. The authors mention that no patients with somatic FAS-ALPS have been diagnosed with lymphoma and wisely point out that they are probably at risk and should be monitored carefully. Holzeva and colleagues surmised that somatic FAS-ALPS is not a premalignant state because TCR gene rearrangements were oligoclonal or polyclonal in the small subset they studied.2 Whereas TCR gene rearrangement analysis is helpful in establishing clonality, further research is needed to determine whether somatic FAS-ALPS is a clonal disease. Clonal early lineage T-cell populations can produce polyclonal circulating T cells. A correlative example is T-lineage myelodysplastic syndrome that can have polyclonal TCR rearrangements, yet have clonal cytogenetic abnormalities. Hypothetically, in somatic FAS-ALPS, the mutation may arise in a T-cell clone that produces polyclonal DNTs. Nevertheless, clonality does not necessarily equate to malignancy, as patients with Epstein-Barr virus infections can develop monoclonal expansion of T cells that resolve spontaneously. Further investigation and prospective monitoring of these patients is needed.
A final lingering question that the study of somatic FAS-ALPS may help answer is whether DNTs drive the disease or are merely an epiphenomenon. If the mutation in FAS is localized to the DNT compartment, and patients develop the same phenotype as those with germline mutations, it suggests the DNTs drive the disease as they are the only affected cell. Recent work suggests DNTs are the drivers and not bystanders in lupus patients.7 In summary, Dowdell et al have made a number of key observations in a poorly studied ALPS variant that can potentially change the understanding of ALPS pathophysiology and clinical practice.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal