Abstract
The survival of young children with sickle cell disease (SCD) has improved, but less is known about older children and adolescents. We studied the Dallas Newborn Cohort (DNC) to estimate contemporary 18-year survival for newborns with SCD and document changes in the causes and ages of death over time. We also explored whether improvements in the quality of medical care were temporally associated with survival. The DNC now includes 940 subjects with 8857 patient-years of follow-up. Most children with sickle cell anemia (93.9%) and nearly all children with milder forms of SCD (98.4%) now live to become adults. The incidence of death and the pattern of mortality changed over the duration of the cohort. Sepsis is no longer the leading cause of death. All the recent deaths in the cohort occurred in patients 18 years or older, most shortly after the transition to adult care. Quality of care in the DNC has improved over time, with significantly more timely initial visits and preventive interventions for young children. In summary, most children with SCD now survive the childhood years, but young adults who transition to adult medical care are at high risk for early death.
Introduction
Sickle cell disease (SCD) is a group of genetic disorders of hemoglobin that causes multisystem morbidity and an increased risk of early death. The survival of young children with SCD has improved dramatically over the past several decades.1-3 Newborn screening, prophylactic penicillin, and effective vaccinations against Haemophilus influenzae type b and Streptococcus pneumoniae are believed to be largely responsible for the marked decrease in mortality during early childhood.4-6 Indeed, in our initial report of the Dallas Newborn Cohort (DNC) in 2004, we estimated that 95% of children with sickle cell anemia (HbSS), the most severe form of SCD, survive the first decade of life.2
Less is known about the outcome of older children and adolescents with SCD given contemporary care. We do not know the proportion of children born in the United States with SCD who survive until adulthood. Perhaps improvements in early survival have simply shifted the burden of mortality to later childhood. In our initial report of the DNC, we estimated the rate of survival at age 18 years to be only 85.6% (95% confidence interval [CI]: 73.4-97.8) for children with sickle cell anemia (HbSS).2 This estimate was inexact with a wide confidence interval because only 9 cohort subjects were 18 years or older at the time of analysis.
Although survival has improved, especially for young children with SCD, we do not know all the reasons for this progress. Only one of the interventions believed to have improved survival, prophylactic penicillin, has been formally tested in a clinical trial.4 Less is known about the impact of other interventions. For example, immunizations have decreased the incidence of invasive pneumococcal infections,7,8 but the association between immunization status and survival has not been explored in a SCD newborn cohort. We also do not know whether survival is associated with the quality of medical care delivered to children with SCD, such as the timely institution of interventions to decrease pneumococcal infections.
Therefore, we studied the DNC to provide a contemporary estimate of 18-year survival for newborns with SCD and document the changes in the causes and timing of death over time. We also explored whether improvements in quality of medical care were temporally associated with survival. Specifically, we studied the timeliness of the initiation of prophylactic penicillin, the initial visit to our sickle cell center, and the administration of vaccinations against the pneumococcus. We hypothesized that survival has improved over the duration of the DNC, and that the burden of mortality had shifted to adolescents and young adults.
Methods
Description of the cohort
The DNC is a newborn inception cohort that comprises the children we follow in our tertiary care center who were diagnosed with SCD at birth by newborn screening for hemoglobinopathies in Texas beginning in 1983.2 The DNC includes children with the 4 main genotypes of SCD: HbSS, sickle hemoglobin C disease (HbSC), sickle β+-thalassemia (HbSβ+), and sickle β0-thalassemia (HbSβ0). Subjects are tracked prospectively in our center's clinical SCD database, which has been computer based since 1982 (preceding the inception of the cohort). We continuously update the status and clinical information on subjects at each clinical encounter. The Institutional Review Board of the University of Texas Southwestern Medical Center approved the use of the clinical database for this project and waived the requirement for written informed consent.
Cohort members with HbSS and HbSβ0 have been uniformly prescribed prophylactic penicillin until at least age 5 years since the inception of the cohort. Our center's policy is to immunize all children with SCD with 2 doses of the 23-valent pneumococcal polysaccharide vaccine (PPV-23; Pneumovax; Merck & Co, Inc) at 2 and 5 years of age. After the licensure of the heptavalent-conjugated pneumococcal vaccine (PCV-7; Prevnar; Wyeth Pharmaceuticals) in 2000, our policy has been to ensure that all infants with SCD receive 4 doses of PCV-7, according to the guidelines of the American Academy of Pediatrics.9 For older children who did not receive PCV-7 in infancy, we administer 2 doses of PCV-7 at least 2 months apart for those younger than 5 years and 1 dose for those 5 years or older.
We systematically contact patients and families who do not keep clinic appointments. After the first missed appointment, a patient is automatically rescheduled and notified of the new appointment. After the second and third consecutive no-show, the sickle cell social worker contacts the family to determine the reasons for missed appointments and provides needed assistance. After the fourth consecutive no-show, a certified letter is sent to the family notifying them of the need to maintain follow-up and how to contact our center.
We transfer patients to adult sickle cell care programs at 18 years of age. We provide education and guidance throughout childhood and adolescence, but the formal transition process begins at 17 years of age. We provide verbal and written information about our affiliated sickle cell program for adults, which is on the same campus as our pediatric program, as well as about providers in the community. During their last visit with us at 18 years of age, we facilitate their first appointment with an adult provider. Adult patients and program personnel meet the transitioning patient at this final visit when possible. We provide care for patients until they make their first clinic visit with an adult provider. There is no systematic follow-up of these older patients in our pediatric program or database. However, we record all the deaths we learn about from communication with families or adult medical providers.
Definitions and outcomes
We classified the status of each patient as: (1) active—evaluated in our center within the past 2 years; (2) inactive—last evaluated in our center 2 to 5 years ago; (3) lost to follow-up—not evaluated in more than 5 years; (4) moved; (5) deceased; or (6) transitioned to adult medical care. The designation of active, inactive, and lost to follow-up are based only on clinic visits and hospitalizations in our pediatric center. Telephone contact or evaluations at other medical facilities do not fulfill the criteria for these categories.
We identified all known deaths in the cohort by query of the database. We further cross-referenced the newborn screening follow-up database maintained by the Texas Department of State Health Services to identify any deaths of which we may have been unaware. Deaths were classified by age and cause of death. Cause of death was subclassified as SCD related or not.2 This analysis represents follow-up from the inception of the cohort in 1983 through August 1, 2007.
We prospectively defined 4 measures of quality medical care for young children with SCD: (1) age at initiation of prophylactic penicillin (for HbSS and HbSβ0 subjects only, because we do not systematically prescribe it for other genotypes); (2) age at first visit to our sickle cell center; (3) age at first dose of PCV-7; and (4) age at first dose of PPV-23. We aim to start prophylactic penicillin for HbSS and HbSβ0 subjects and evaluate all infants identified by newborn screening to have SCD by 2 months of age. We also aim to administer (or ensure the administration by another health care provider) the first doses of PCV-7 and PPV-23 by 2 months and 2 years (24 months) of age, respectively. To allow for some variation in practice due to issues such as transportation, referral from primary care providers, and scheduling of clinic appointments, we considered the quality measures to have been satisfied if a subject was first prescribed prophylactic penicillin, evaluated in our center, and given the first dose of PCV-7 by 90 days of age. The PPV-23 measure was satisfied if the first dose was given by 3 years (36 months) of age.
Statistical analysis
Summary statistics were computed for variables of interest. The Fisher exact or χ2 tests were used to compare 2 or 3 or more proportions, respectively. We estimated overall survival at 18 years of age by the Kaplan-Meier method. Entry into the cohort was defined as the date of birth. Surviving subjects were censored on the date of their last clinic visit or hospitalization at our center through August 1, 2007. We did not censor any period of observation for patients who received hydroxyurea, chronic transfusion therapy, or stem cell transplant, because we aimed to measure the impact on survival of all contemporary therapies, from prophylactic penicillin to transplantation. We also divided the cohort into 3 roughly equal “eras” based on the year of birth of each subject (1983-1990, 1991-1999, and 2000-2007) to explore trends in survival by birth era over the 25 years of follow-up currently provided by the DNC. We also compared the survival data of the DNC to other published cohorts of children with SCD. Published survival curves from the infant cohort of the Cooperative Study of Sickle Cell Disease (CSSCD)10 and the Jamaican sickle cell cohort3 were digitized, the survival estimates were deduced from (x,y) coordinates, and the curves were redrawn for comparison to the DNC. Dr Paul Telfer (Barts and The London School of Medicine and Dentistry) provided the survival data for the East London cohort.11
We used 1-way analysis of variance and a posttest for linear trend to identify any linear relationship between year of birth and mean age at (a) initiation of penicillin, (b) first visit to our center, (c) first dose of PCV-7, and (d) first dose of PPV-23. We also tested for differences in the median age at initiation of penicillin, first visit, and first doses of PCV-7 and PPV-23 by year of birth using Kruskal-Wallis analysis of variance with Dunn posttest. Incidence of death (all-cause) was calculated per 100 patient-years of observation for the HbSS and HbSβ0 group and the HbSC and HbSβ+ group separately.
We analyzed data and generated figures with PASW Version 18.0 statistical software for Mac (SPSS) and GraphPad Prism 5.0c for Mac (GraphPad Software). A P value of less than .05 was considered statistically significant; no correction was made for multiple statistical comparisons.
Results
Current characteristics of the cohort
The DNC now includes 940 subjects and provides 8857 patient-years of follow-up (Table 1). Mean follow-up is 9.4 years (median, 9.2 years; range, 0.08-20.6 years). This is an increase of 229 subjects and 3201 patient-years of follow-up since the original publication of the DNC in 2004, which included follow-up through August 1, 2002.2 The status of subjects is shown in Table 2. Subjects with HbSC or HbSβ+ were more likely to be lost to follow-up (no contact within the past 5 years) than those with HbSS or HbSβ0 (14.4% vs 3.2%, P < .001). Compared with the original report,2 the proportion of HbSS or HbSβ0 subjects who are inactive or lost to follow-up has remained stable: inactive, 5.6% currently versus 8.0% in the prior report (P = .131); lost to follow-up, 3.2% currently versus 2.5% (P = .576).
Characteristics of the Dallas Newborn Cohort
| Diagnosis . | No. . | % Male . | Patient-years of follow-up . |
|---|---|---|---|
| HbSS | 572 | 52.8 | 5623 |
| HbSC | 284 | 47.5 | 2541 |
| HbSβ+ | 63 | 55.5 | 498 |
| HbSβ0 | 21 | 66.7 | 196 |
| Total | 940 | 51.8 | 8857 |
| Diagnosis . | No. . | % Male . | Patient-years of follow-up . |
|---|---|---|---|
| HbSS | 572 | 52.8 | 5623 |
| HbSC | 284 | 47.5 | 2541 |
| HbSβ+ | 63 | 55.5 | 498 |
| HbSβ0 | 21 | 66.7 | 196 |
| Total | 940 | 51.8 | 8857 |
HbSS indicates sickle cell anemia; HbSC, sickle hemoglobin C disease; HbSβ+, sickle β+-thalassemia; and HbSβ0, sickle β0-thalassemia.
Status of subjects in the Dallas Newborn Cohort
| Status . | Total . | HbSS and HbSβ0 . | HbSC and HbSβ+ . | |||
|---|---|---|---|---|---|---|
| No. . | % . | No. . | % . | No. . | % . | |
| Active: evaluated within the past 2 y | 499 | 53 | 337 | 56.8 | 161 | 46.4 |
| Inactive: last evaluated 2-5 y ago | 76 | 8.1 | 33 | 5.6 | 44 | 12.7 |
| Lost to follow-up: not evaluated in 5 or more y | 69 | 7.3 | 19 | 3.2 | 50 | 14.4 |
| Moved | 64 | 6.8 | 46 | 7.8 | 18 | 5.2 |
| Deceased | 32 | 3.4 | 29 | 4.9 | 3 | 0.9 |
| Transitioned to adult care | 201 | 21.4 | 129 | 21.8 | 71 | 20.5 |
| Status . | Total . | HbSS and HbSβ0 . | HbSC and HbSβ+ . | |||
|---|---|---|---|---|---|---|
| No. . | % . | No. . | % . | No. . | % . | |
| Active: evaluated within the past 2 y | 499 | 53 | 337 | 56.8 | 161 | 46.4 |
| Inactive: last evaluated 2-5 y ago | 76 | 8.1 | 33 | 5.6 | 44 | 12.7 |
| Lost to follow-up: not evaluated in 5 or more y | 69 | 7.3 | 19 | 3.2 | 50 | 14.4 |
| Moved | 64 | 6.8 | 46 | 7.8 | 18 | 5.2 |
| Deceased | 32 | 3.4 | 29 | 4.9 | 3 | 0.9 |
| Transitioned to adult care | 201 | 21.4 | 129 | 21.8 | 71 | 20.5 |
HbSS, sickle cell anemia; HbSβ0, sickle β0-thalassemia; HbSC, sickle hemoglobin C disease; and HbSβ+, sickle β+-thalassemia.
Mortality
The causes of all 32 known deaths are shown in Table 3. We identified no deaths of which we were unaware in the newborn screening follow-up database maintained by the Texas Department of State Health Services. All deaths known to be caused, even partly, by bacterial sepsis are classified only as sepsis for this analysis. One death originally classified as trauma2 is reclassified here as SCD related, because the archived medical records revealed that the patient died of acute chest syndrome after a motor vehicle collision. All deaths in the HbSC and HbSβ+ group were not clearly related to SCD.
Deaths in the Dallas Newborn Cohort
| Cause of death . | No. . | Age at death, y . |
|---|---|---|
| Probably related to SCD | 23 | |
| Acute chest syndrome | 5 | 4, 5, 5, 18, 19 |
| Multiorgan failure syndrome | 4 | 4, 14, 18, 19 |
| Pneumococcal sepsis | 4 | 2, 3, 5, 5 |
| Multifactorial or unknown | 4 | <1, 2, 4, 20 |
| H influenzae type b sepsis | 1 | 1 |
| Myocardial infarction | 1 | 13 |
| Complications of recurrent stroke | 1 | 7 |
| Neurologic event | 1 | 23 |
| Complications of renal failure | 1 | 18 |
| Ceftriaxone-induced hemolysis | 1 | 2 |
| Probably unrelated to SCD | 9 | |
| Trauma | 2 | 1,* 17 |
| Glutaric acidemia type 2 | 1 | 12 |
| Down, Hirschsprung, CHD | 1 | 5 |
| Acute viral myocarditis | 1 | 1 |
| Drowning | 1 | 1 |
| Complex CHD | 1 | 1 |
| γδ-T-cell lymphoma | 1 | 12* |
| Other metabolic disorder | 1 | 1† |
| Cause of death . | No. . | Age at death, y . |
|---|---|---|
| Probably related to SCD | 23 | |
| Acute chest syndrome | 5 | 4, 5, 5, 18, 19 |
| Multiorgan failure syndrome | 4 | 4, 14, 18, 19 |
| Pneumococcal sepsis | 4 | 2, 3, 5, 5 |
| Multifactorial or unknown | 4 | <1, 2, 4, 20 |
| H influenzae type b sepsis | 1 | 1 |
| Myocardial infarction | 1 | 13 |
| Complications of recurrent stroke | 1 | 7 |
| Neurologic event | 1 | 23 |
| Complications of renal failure | 1 | 18 |
| Ceftriaxone-induced hemolysis | 1 | 2 |
| Probably unrelated to SCD | 9 | |
| Trauma | 2 | 1,* 17 |
| Glutaric acidemia type 2 | 1 | 12 |
| Down, Hirschsprung, CHD | 1 | 5 |
| Acute viral myocarditis | 1 | 1 |
| Drowning | 1 | 1 |
| Complex CHD | 1 | 1 |
| γδ-T-cell lymphoma | 1 | 12* |
| Other metabolic disorder | 1 | 1† |
CHD indicates congenital heart disease.
Sickle hemoglobin C disease.
Sickle β+-thalassemia.
All of the 7 new deaths since the initial analysis (with follow-up through August 1, 2002)2 occurred in subjects who were 18 years or older (Table 4). Of these 7 deaths, 6 occurred after the patient was transferred to adult medical care. Only 1 was known to have an overt, chronic complication of SCD. The mean time between transfer to adult care and death was 1.8 years (median, 1.2 years; range, 0.2-5.3 years). The highest incidence of death in the DNC is now in patients 15 years or older, which is at least 3 times the incidence in other, younger age groups (Table 5). Consequently, the age at death in the DNC has increased by calendar year of death: the median age of death was 3.0 years for deaths that occurred in 1983 to 1990, 3.1 years for 1991 to 2000, and 17.1 years for 2001 to 2007 (P = .001).
Circumstances of death in patients 18 years or older and the relationship to transition to adult care
| Patient no. . | Age at transition, y . | Age at death, y . | Chronic complication of sickle cell disease . | Circumstances of death . |
|---|---|---|---|---|
| 1 | N/A* | 18.8 | Renal failure; dialysis | Found dead at home |
| 2 | 17.9 | 19.2 | None known | Acute chest syndrome |
| 3 | 18.0 | 18.3 | None known | Acute chest syndrome−refused transfusion (Jehovah's Witness) |
| 4 | 18.2 | 20.6 | None known | Fell in hospital while pregnant−cerebral hemorrhage |
| 5 | 18.3 | 19.3 | None known | Acute chest syndrome complicated by multiorgan failure syndrome |
| 6 | 18.4 | 23.7 | None known | Presumed stroke† |
| 7 | 18.5 | 18.7 | None known | Multiorgan failure syndrome |
| Patient no. . | Age at transition, y . | Age at death, y . | Chronic complication of sickle cell disease . | Circumstances of death . |
|---|---|---|---|---|
| 1 | N/A* | 18.8 | Renal failure; dialysis | Found dead at home |
| 2 | 17.9 | 19.2 | None known | Acute chest syndrome |
| 3 | 18.0 | 18.3 | None known | Acute chest syndrome−refused transfusion (Jehovah's Witness) |
| 4 | 18.2 | 20.6 | None known | Fell in hospital while pregnant−cerebral hemorrhage |
| 5 | 18.3 | 19.3 | None known | Acute chest syndrome complicated by multiorgan failure syndrome |
| 6 | 18.4 | 23.7 | None known | Presumed stroke† |
| 7 | 18.5 | 18.7 | None known | Multiorgan failure syndrome |
Not applicable: transition delayed beyond 18 years of age because of chronic renal failure.
This was the first patient in the Dallas Newborn Cohort.
Incidence of death among HbSS and HbSβ0 patients by cohort era
| Age group, y . | Era 1: 1983-1990 . | Era 2: 1991-1999 . | Era 3: 2000-2007 . |
|---|---|---|---|
| 0-1.99 | 0.50 | 0.72 | 0.32 |
| 2-4.99 | 0.73 | 0.35 | 0 |
| 5-9.99 | 0.34 | 0.37 | 0 |
| 10-14.99 | 0.38 | 0 | |
| 15 or older | 2.00 | ||
| Overall | 0.67 | 0.37 | 0.15 |
| Age group, y . | Era 1: 1983-1990 . | Era 2: 1991-1999 . | Era 3: 2000-2007 . |
|---|---|---|---|
| 0-1.99 | 0.50 | 0.72 | 0.32 |
| 2-4.99 | 0.73 | 0.35 | 0 |
| 5-9.99 | 0.34 | 0.37 | 0 |
| 10-14.99 | 0.38 | 0 | |
| 15 or older | 2.00 | ||
| Overall | 0.67 | 0.37 | 0.15 |
Incidence rates are expressed as the number of deaths per 100 patient-years.
The use of the protein-conjugate vaccines against H influenzae type b and the pneumococcus (PCV-7) appear to have changed the patterns of mortality over the duration of the cohort (Figure 1). Prophylactic penicillin in combination with PPV-23 (both used since 1983 in the DNC) was not sufficient to prevent fatal pneumococcal infection, but the introduction of PCV-7 in 2000 was temporally associated with a marked decrease and possible elimination of such deaths in our cohort. Acute chest syndrome and multiorgan failure syndrome have now surpassed bacterial sepsis as the leading causes of death in the DNC (Table 3; Figure 1).
Temporal changes in causes of death in children with sickle cell disease. Three categories of death are shown on the y-axis: deaths due to acute chest syndrome (ACS) and multiorgan failure syndrome (MOFS), deaths due to sepsis, and deaths of all other causes. Together, deaths due to ACS and MOFS are now more common than fatal sepsis. Notably, no member of the cohort has died from Haemophilus influenzae type b sepsis ( ) or Streptococcus pneumoniae sepsis (
) or Streptococcus pneumoniae sepsis ( ) since the availability of the protein-conjugate vaccine against either bacterium (dotted lines).
) since the availability of the protein-conjugate vaccine against either bacterium (dotted lines).
Temporal changes in causes of death in children with sickle cell disease. Three categories of death are shown on the y-axis: deaths due to acute chest syndrome (ACS) and multiorgan failure syndrome (MOFS), deaths due to sepsis, and deaths of all other causes. Together, deaths due to ACS and MOFS are now more common than fatal sepsis. Notably, no member of the cohort has died from Haemophilus influenzae type b sepsis ( ) or Streptococcus pneumoniae sepsis (
) or Streptococcus pneumoniae sepsis ( ) since the availability of the protein-conjugate vaccine against either bacterium (dotted lines).
) since the availability of the protein-conjugate vaccine against either bacterium (dotted lines).
The overall incidence of death (all-cause mortality) in the DNC is now 0.52 deaths/100 patient-years for HbSS and HbSβ0 patients and 0.10 for HbSC and HbSβ+ patients. These compare with 0.59 and 0.24, respectively, in our original report.2 The frequency of death for HbSS and HbSβ0 patients has decreased by cohort era: 20 of 198 subjects born in 1983 to 1990, 8 of 215 subjects born in 1991 to 2000, and 1 of 180 subjects born in 2001 to 2007 (P < .001). This corresponds to an incidence of death (all-cause mortality) of 0.67, 0.37, and 0.15/100 patient-years of follow-up, respectively, for each cohort era (Figure 2C). The 3 cohort eras have different age compositions, and the incidence of death by age group across cohort eras is shown in Table 5.
Survival of children with sickle cell disease. (A) Overall survival (all-cause mortality) for children with sickle cell anemia and sickle β0-thalassemia. Estimated survival at 18 years of age is 93.9% (95% CI: 90.3-96.2). Numbers above the x-axis indicate the number of subjects at risk at each age. (B) Overall survival (all-cause mortality) for children with sickle hemoglobin C disease and sickle β+-thalassemia. Estimated survival at 18 years of age is 98.4% (95% CI: 94.4-99.5). Numbers above the x-axis indicate the number of subjects at risk at each age. (C) Trends in overall survival for children with sickle cell anemia and sickle β0-thalassemia by cohort era. Cohort eras are defined by year of birth (1983-1990, 1991-1999, and 2000-2007). (D) Comparison of overall survival for children with sickle cell anemia and sickle β0-thalassemia by cohort. We compare the first and last thirds of the Jamaican cohort, the infant cohort of the Cooperative Study of Sickle Cell Disease, the East London Cohort, and the first and last eras of the Dallas Newborn Cohort. Note that the y-axes (fraction surviving) of all panels do not begin at 0.
Survival of children with sickle cell disease. (A) Overall survival (all-cause mortality) for children with sickle cell anemia and sickle β0-thalassemia. Estimated survival at 18 years of age is 93.9% (95% CI: 90.3-96.2). Numbers above the x-axis indicate the number of subjects at risk at each age. (B) Overall survival (all-cause mortality) for children with sickle hemoglobin C disease and sickle β+-thalassemia. Estimated survival at 18 years of age is 98.4% (95% CI: 94.4-99.5). Numbers above the x-axis indicate the number of subjects at risk at each age. (C) Trends in overall survival for children with sickle cell anemia and sickle β0-thalassemia by cohort era. Cohort eras are defined by year of birth (1983-1990, 1991-1999, and 2000-2007). (D) Comparison of overall survival for children with sickle cell anemia and sickle β0-thalassemia by cohort. We compare the first and last thirds of the Jamaican cohort, the infant cohort of the Cooperative Study of Sickle Cell Disease, the East London Cohort, and the first and last eras of the Dallas Newborn Cohort. Note that the y-axes (fraction surviving) of all panels do not begin at 0.
Survival
For HbSS and HbSβ0 patients, we now estimate overall survival at 18 years of age to be 93.9% (95% CI: 90.3-96.2; Figure 2A). This point estimate is more exact than, and suggestive of an improvement from, the 85.6% (95% CI: 73.4-94.8) estimate in the initial publication of the cohort.2 For HbSC and HbSβ+ patients, we now estimate overall survival at 18 years of age to be 98.4% (95% CI: 94.4-99.5; Figure 2B), compared with 97.4% (95% CI: 93.9-100) in the initial publication.2 The HbSS and HbSβ0 group continues to have significantly worse overall survival than the subjects with HbSC and HbSβ+ (hazard ratio, 2.8; P = .009). Overall survival for the HbSS and HbSβ0 group appears to improve by cohort era (Figure 2C), and is better than in previous SCD cohorts (Figure 2D). Survival to age 5 years for the HbSS and HbSβ0 group, an indicator of early mortality from sepsis, also appears to have increased by cohort era: 96.8% (1983-1990), 97.5% (1991-2000), and 99.2% (2001-2007).
Quality of medical care
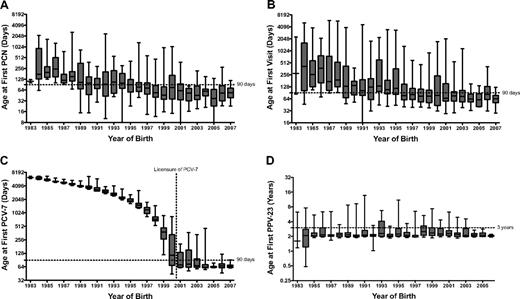
The mean age of initiation of penicillin has decreased significantly since the inception of the DNC (slope = −12.2, r2 = 0.04, P < .001; Figure 3A). The median age at initiation of PCN for the HbSS and HbSβ0 group has decreased from 177 days in 1984 (the first full calendar year of the DNC) to 54 days in 2007 (P < .001), and the proportion of subjects whose age of initiation of penicillin occurred by 90 days of age has increased from 7.1% to 88.9% (P = .001). The mean age of a patient's first visit to our center has decreased significantly since the inception of the DNC (slope = −34.8, r2 = 0.05, P < .001; Figure 3B). The median age at first visit was 415 days in 1984 and 64 days in 2007 (P < .001). Over the same interval, the proportion of subjects whose first visit occurred by 90 days of age has progressively increased from 10% to 84.6% (P < .001).
Measures of quality medical care for children with sickle cell disease. (A) The age when prophylactic penicillin was first prescribed for subjects with sickle cell anemia and sickle β0-thalassemia. (B) The age at first visit to our center by year of birth for all cohort subjects. (C) The age at first dose of 7-valent protein-conjugated pneumococcal vaccine (PCV-7) for all cohort subjects. The time to first PCV-7 in patients born before 2000 reflects only the age of patients at the time the vaccine became available (dotted line), not quality of care. (D) The age at first dose of 23-valent polysaccharide pneumococcal vaccine (PPV-23) for all cohort subjects. For all panels, boxes show the median and the 25th and 75th percentiles, and whiskers show the 5th and 95th percentiles. Note the logarithmic scale (base 2) of the y-axes in all panels.
Measures of quality medical care for children with sickle cell disease. (A) The age when prophylactic penicillin was first prescribed for subjects with sickle cell anemia and sickle β0-thalassemia. (B) The age at first visit to our center by year of birth for all cohort subjects. (C) The age at first dose of 7-valent protein-conjugated pneumococcal vaccine (PCV-7) for all cohort subjects. The time to first PCV-7 in patients born before 2000 reflects only the age of patients at the time the vaccine became available (dotted line), not quality of care. (D) The age at first dose of 23-valent polysaccharide pneumococcal vaccine (PPV-23) for all cohort subjects. For all panels, boxes show the median and the 25th and 75th percentiles, and whiskers show the 5th and 95th percentiles. Note the logarithmic scale (base 2) of the y-axes in all panels.
The mean age of a subject's first dose of PCV-7 has decreased significantly since the licensure of the vaccination in 2000 (slope = −7.63, r2 = 0.04, P < .018; Figure 3B). The time to first PCV-7 in patients born before 2000 reflects only the age of patients at the time the vaccine became available. Therefore, for this quality measure, we considered only patients born after 2000. The median age at first dose of PCV-7 and the proportion of patients who received their first dose by 90 days of age have improved from 71 days and 68.4%, respectively, in 2001 to 65 days and 90%, respectively, in 2007. There has been no linear decrease in time of first PPV-23 since the inception of the cohort (slope = −0.008, r2 = 0.004, P = .155; Figure 3D), and median age at the time of first dose of PPV-23 has remained relatively stable at approximately 2.0 years (24 months). However, the variability in the time of the first dose of PPV-23 appears to have decreased. The proportion of subjects who received their first dose of PPV-23 by 3 years of age has also remained relatively stable (82.4% in 1994 vs 100% in 2006; P = .238). Subjects born in 2007 and the latter part of 2006 were too young to have received PPV-23 at the time of this analysis.
Discussion
Most children with HbSS or HbSβ0 (93.9%) and nearly all children with HbSC or HbSβ+ (98.4%) now live to become adults. Acute chest syndrome and multiorgan failure syndrome have now surpassed bacterial sepsis as the leading cause of death in the DNC. The combination of prophylactic penicillin and immunization with PPV-23 was not sufficient to prevent all fatal pneumococcal infections, but the addition of the PCV-7 in 2000 appears to have eliminated such deaths to date. Concurrent with the improvement in survival we also documented an improvement in the quality of care for children with SCD, as indicated by more timely initiation of prophylactic penicillin, first visit to our sickle cell center, and initial vaccinations against the pneumococcus. Finally, we show that young adults, shortly after the transition to adult medical care, seem to be at high risk for death.
Universal newborn screening for hemoglobinopathies and prophylactic penicillin likely explains some of the improvement in survival in the DNC compared with the CSSCD infant cohort10 and the Jamaican sickle cell cohort (Figure 2D).3 Other contributory factors may include new medical therapeutics, improved supportive care during acute “crises,” and better quality of medical care. It has become increasingly difficult to explore these possibilities by comparing the DNC with historical cohorts (eg, CSSCD) or cohorts in markedly different socioeconomic settings (eg, Jamaica). The East London sickle cell cohort11 is contemporary and similar to the DNC in design and socioeconomic setting. Although much smaller than the DNC (1517 vs 5623 patient-years of follow-up for HbSS subjects), the East London cohort also reports excellent survival for patients with HbSS: 99.0% at 20 years (95% CI: 93.2-99.9; Figure 2D).11 This is similar to our finding of 93.9% at 18 years (95% CI: 90.3-96.2). A comparison of other well-characterized cohorts in developed countries is now needed to explore potential differences in medical management, quality of care, and health policies that may affect patient outcomes.
Our report provides contemporary survival data for children with SCD that can facilitate the treatment and counseling of patients and their families, guide public health interventions, and provide the foundation for future research. To our knowledge, we are the first to report a systematic study of measures of quality care over time in children with SCD and correlate these findings with trends in survival. Current and future cohorts should incorporate such measures into their design, especially as death is now, fortunately, an uncommon outcome in childhood. We also confirm that the burden of mortality is increasingly shifting to adults, and that the transition from pediatric to adult medical care appears to be a high-risk period for death. Young adults are an especially vulnerable population with a high risk of mortality at the imperfect interface between pediatric and adult medical care.12 Our results argue for a need to better link pediatric and adult programs, perhaps by creating special clinics for adolescents and young adults run jointly by pediatric and adult medical providers with expertise in SCD. Because many of the deaths we observed after transition occurred in the context of acute medical events, young adults also need a clearly identified center with expertise in SCD for acute medical care.
Our study has several limitations. First, although we have shown a temporal correlation between improving survival and quality of medical care, we cannot conclude a causal correlation in a cohort study. Second, we did not study other measures of quality care that may also affect survival, such as parental education about the importance of fever or parental competence in splenic palpation.13 We studied only a limited number of practical, easily defined, quantitative markers of quality of care relevant to care in early childhood. Third, we analyzed only the time to initial pneumococcal vaccination, not the completion of the series. We chose this approach because it better reflects early intervention. It also maximizes the amount of data to analyze, as younger children (< 5 years of age) will not yet have received their second dose of PPV-23, and it simplifies the analysis, because a “complete” series of the PCV-7 can be achieved in different ways depending on the child's age. Fourth, we did not evaluate concurrent interventions, such as increased use of hydroxyurea14 or chronic red blood cell transfusions,15 that could also affect survival. Although further research to define other factors associated with improving survival is clearly needed, we are the first to systematically study selected measures of quality care over time in a SCD cohort. Finally, the limitations that are inherent to the design of the DNC, including the dependence on referral by a primary care provider to our center and loss to follow-up, have been described previously.2 The loss to follow-up rates in the DNC are driven mainly by the HbSC/HbSβ+ subgroup, patients known to have lower SCD-related morbidity and mortality. Thus, death is not likely to be the main reason for loss to follow-up. Moreover, for purposes of survival analysis, we do not assume that patients are alive or dead after their last contact in our center. We believe our findings can be generalized to children with SCD who are cared for in developed nations at specialized centers with pediatric hematologists.
In summary, most children with SCD now survive the childhood years, and the burden of mortality has shifted to young adults. The transition from pediatric to adult medical care appears to be a high-risk period for mortality. Young adults urgently need the high-quality medical care and systematic follow-up that have been available to children to continue to improve the life expectancy of people with SCD.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Nancy J. Lee, Kimberly Thomas, and Sandra Richardson for their assistance with the collection of data and the staff of the Newborn Screening Program of the Texas Department of State Health Services for their unbridled enthusiasm, professionalism, and dedication these past 25 years to the early diagnosis and follow-up of children in our state with sickle cell disease.
This work was supported in part by grants from the National Institutes of Health (U54-HL70588, KL2-RR024983).
National Institutes of Health
Authorship
Contribution: C.T.Q. designed the research, oversaw the data collection, performed the statistical analysis, and wrote the paper; and T.L.M., Z.R.R., and G.R.B. assisted in study design, analysis, and writing of the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Charles T. Quinn, UT Southwestern Medical Center, 5323 Harry Hines Blvd, Dallas, TX 75390-9063; e-mail: charlestquinn@gmail.com.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal