Abstract
On the path to successful immunotherapy of hematopoietic tumors, γδ T cells offer great promise because of their human leukocyte antigen (HLA)–unrestricted targeting of a wide variety of leukemias/lymphomas. However, the molecular mechanisms underlying lymphoma recognition by γδ T cells remain unclear. Here we show that the expression levels of UL16-binding protein 1 (ULBP1) determine lymphoma susceptibility to γδ T cell–mediated cytolysis. Consistent with this, blockade of NKG2D, the receptor for ULBP1 expressed on all Vγ9+ T cells, significantly inhibits lymphoma cell killing. Specific loss-of-function studies demonstrate that the role of ULBP1 is nonredundant, highlighting a thus far unique physiologic relevance for tumor recognition by γδ T cells. Importantly, we observed a very wide spectrum of ULBP1 expression levels in primary biopsies obtained from lymphoma and leukemia patients. We suggest this will impact on the responsiveness to γδ T cell–based immunotherapy, and therefore propose ULBP1 to be used as a leukemia/lymphoma biomarker in upcoming clinical trials.
Introduction
Cellular immunotherapy of hematopoietic malignancies is regarded as one of the most promising approaches to deal with the common relapse or resistance to conventional treatments. γδ T cells are innate-like lymphocytes capable of potent antitumor activity toward a variety of malignant cell types in both mice1 and humans,2 with special emphasis on lymphomas and leukemias.3 Unlike their αβ counterparts, γδ T cells are not restricted by classic major histocompatibility complex (MHC) presentation but share many characteristics with NK cells, including the expression of “NK receptors,” most notably NKG2D.4,5 Most (60%-95%) human γδ peripheral blood lymphocytes (γδ-PBLs) express a Vγ9Vδ2 T-cell receptor (TCR)6 and are specifically activated by nonpeptidic prenyl pyrophosphate intermediates of isoprenoid biosynthesis (“phosphoantigens”),7,8 which constitutes the basis of current cancer immunotherapy strategies involving γδ T cells.2,9,10
Although several molecules have been proposed to play a role in tumor-Vγ9Vδ2 cell interactions, from phosphoantigens7,11 to an F1-ATPase-related structure complexed with delipidated apolipoprotein A-I12 and, more recently, DNAM-1 ligands13 or the nonclassic MHC protein ULBP4,14 a consensus about γδ T-cell recognition of tumors, particularly on physiologic (nonectopic) conditions, is yet to be reached.
Here we set out to determine the mechanism of leukemia/lymphoma cell recognition by γδ T cells, particularly relevant as previous γδ T cell–based clinical trials have shown a variable degree of success among patients.9 The establishment of an in vitro model representative of this clinical scenario and the quantification and manipulation of candidate gene expression allowed us to demonstrate a nonredundant role for ULBP1 in determining the susceptibility of leukemia/lymphoma cells to γδ T cell–mediated cytolysis.
Methods
Cell culture
Peripheral blood mononuclear cell (PBMC) isolation, Vγ9Vδ2 PBL expansion, leukemia/lymphoma cell line cultures, and killing assays were performed as previously described.8
Leukemia/lymphoma biopsies
Pediatric B- or T-cell acute lymphoblastic leukemia cells were obtained from peripheral blood of patients after informed consent and institutional review board approval (Instituto Português de Oncologia, Lisbon, Portugal) in accordance with the Declaration of Helsinki. Lymphoma cells from lymph node biopsies were frozen in liquid nitrogen and used on diagnosis (Hospital de Santa Maria-CHLN, Lisbon, Portugal).
Quantitative RT-PCR
RNA extraction and quantitative reverse-transcribed polymerase chain reaction (RT-PCR) were performed as described,8 using the primers listed in supplemental Table 1 (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Antibodies
The following anti–human monoclonal antibodies were used: ULBP-1/clone IC1380F, MHC class I chain-related gene A (MICA)/clone 1300 (R&D Systems), NKG2D-PE/clone 1D11 (BioLegend), TCRγδ/clone B1.1 (eBioscience), and TCRγδ/clone IMMU510 (Beckman Coulter). Goat anti–mouse IgG-PE (Sigma-Aldrich) was used as secondary monoclonal antibody for ULBP1 and MICA staining.
RNA interference and overexpression
Lentiviral vectors expressing short hairpin RNA (shRNA) for the specific silencing of ULBP1 (CCTGGGAAGAACAAACTGAAA) and MICA (CTATGTCCGTTGTTGTAAGAA) were obtained from the RNAi Consortium and produced as previously described.15 For overexpression of ULBP1, its coding sequence was amplified from a human EST clone (GenBank accession no. BC03541616 ) by PCR, cloned into pENTR-V5C2 vector, subcloned into pLenti6.2 (Invitrogen), and introduced into the Gateway System (Invitrogen). Lentiviruses were then pseudotyped as described.15
Results and discussion
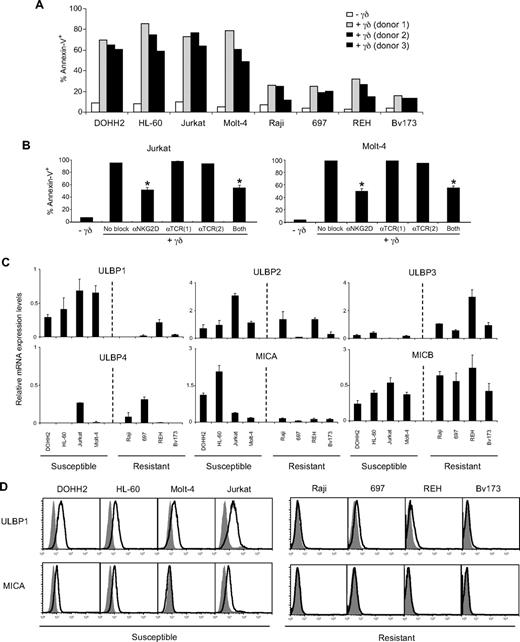
γδ-PBLs, expanded and activated (∼ 100% CD69+; data not shown) with 4-hydroxy-3-methyl-but-2-enylpyrophosphate (HMB-PP), the most potent Vγ9Vδ2 TCR agonist yet known,7,8,17 were able to mediate efficient killing of only a fraction of leukemia/lymphoma cell lines within a large panel established in our laboratory. Within the group selected for this study (supplemental Table 2), 4 lines were highly susceptible (60%-85% annexin V+), whereas the other 4 lines were largely resistant (15%-30% annexin V+) to γδ T-cell cytotoxicity (Figure 1A). Furthermore, we observed a consistent resistance of primary leukemia cells to γδ-PBL cytotoxicity (supplemental Figure 1), which stresses the importance of understanding the mechanisms of tumor cell recognition by γδ T cells.
NKG2D mediates Vγ9Vδ2 T-cell recognition of hematopoietic tumors that endogenously overexpress ULBP1 and MICA. (A) Susceptibility of leukemia and lymphoma cell lines (described in supplemental Table 2) to HMB-PP–activated γδ-PBL (> 90% Vγ9+) cytotoxicity was assessed by coincubating 3 × 104 tumor cells (prelabeled with 1mM DDAO-SE) with 3 × 105 γδ-PBLs from 3 independent donors for 3 hours, then staining with annexin V–fluorescein isothiocyanate and analyzing by flow cytometry. (B) γδ-PBLs were incubated with saturating amounts of anti-NKG2D/clone 1D11 and anti-TCRγδ/clones B1.11 or IMMU5102 blocking antibodies, or both anti-NKG2D and anti-TCRγδ,1 for 1 hour at 4°C. γδ-PBLs were then cocultured either with Jurkat or Molt-4 leukemia lines, and tumor cell lysis was assessed as in panel A. Error bars represent SD (n = 3). *P < .05. (C) Quantitative RT-PCR quantification of mRNA levels of NKG2D ligands in cells lines of panel A, normalized to glucuronidase-β (GUSB) and proteasome subunit β type 6 (PSMB6) housekeeping genes. (D) Flow cytometric analysis of cell-surface expression of ULBP1 and MICA in the leukemia/lymphoma lines of panel A. Data presented in this figure (A-D) are representative of at least 3 independent experiments with consistent results.
NKG2D mediates Vγ9Vδ2 T-cell recognition of hematopoietic tumors that endogenously overexpress ULBP1 and MICA. (A) Susceptibility of leukemia and lymphoma cell lines (described in supplemental Table 2) to HMB-PP–activated γδ-PBL (> 90% Vγ9+) cytotoxicity was assessed by coincubating 3 × 104 tumor cells (prelabeled with 1mM DDAO-SE) with 3 × 105 γδ-PBLs from 3 independent donors for 3 hours, then staining with annexin V–fluorescein isothiocyanate and analyzing by flow cytometry. (B) γδ-PBLs were incubated with saturating amounts of anti-NKG2D/clone 1D11 and anti-TCRγδ/clones B1.11 or IMMU5102 blocking antibodies, or both anti-NKG2D and anti-TCRγδ,1 for 1 hour at 4°C. γδ-PBLs were then cocultured either with Jurkat or Molt-4 leukemia lines, and tumor cell lysis was assessed as in panel A. Error bars represent SD (n = 3). *P < .05. (C) Quantitative RT-PCR quantification of mRNA levels of NKG2D ligands in cells lines of panel A, normalized to glucuronidase-β (GUSB) and proteasome subunit β type 6 (PSMB6) housekeeping genes. (D) Flow cytometric analysis of cell-surface expression of ULBP1 and MICA in the leukemia/lymphoma lines of panel A. Data presented in this figure (A-D) are representative of at least 3 independent experiments with consistent results.
Both TCRγδ and NKG2D have been implicated in Vγ9Vδ2 T cell–mediated killing of epithelial tumors.18–20 To determine their importance in recognition of hematopoietic tumors, we performed specific antibody blockade experiments with HMB-PP–activated γδ-PBL (> 90% Vγ9+) and 2 susceptible leukemia lines. We observed a significant reduction through NKG2D inhibition but not via TCRγδ blockade, and no additive effect (Figure 1B), suggesting that, although TCR-mediated activation greatly augments Vγ9Vδ2 T-cell cytolytic capacity,8 the recognition of leukemia targets is essentially mediated by NKG2D. Moreover, we did not observe any Ca2+ influx in Vγ9Vδ2 T cells during the killing assay (data not shown), which is consistent with TCR-independent tumor cell recognition. Thus, γδ T cell–mediated surveillance of hematopoietic tumors appears to be a 2-step process where effector lymphocyte activation is achieved through TCR stimulation (presumably by endogenous phophoantigens7,11 ) but tumor cell recognition is predominantly mediated by NKG2D.
Based on these results, we hypothesized that the distinct leukemia/lymphoma susceptibilities were derived from differential expression of NKG2D-ligand(s) (NKG2DL), which was tested by quantitative RT-PCR. ULBP1 expression clearly segregated the best with susceptible versus resistant leukemias/lymphomas; on average, ULBP1 mRNA expression was 6-fold higher in susceptible than in resistant lines (Figure 1C). MICA was also highly expressed in some but not all susceptible lines, whereas ULBP3 was enriched in some resistant cell lines, and the expression of the other NKG2DL did not segregate with susceptibility to γδ-mediated killing (Figure 1C). Of note, ULBP4, recently suggested to be involved in γδ-PBL targeting of some epithelial tumors,14 was very poorly expressed in leukemias/lymphomas (Figures 1C, 2D-E). We also confirmed by flow cytometry that ULBP1 and MICA were differentially expressed at the protein level and on the cell surface, although the correlation between mRNA and protein expression was not absolute (Figure 1D).
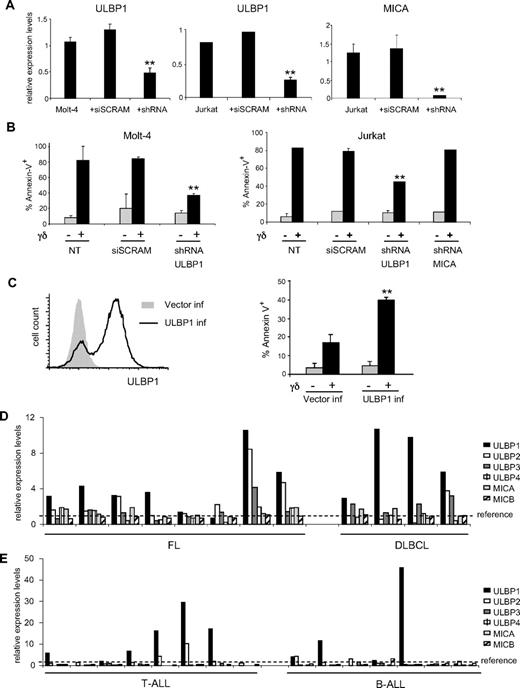
ULBP1 is required for Vγ9Vδ2 T-cell recognition of leukemia/lymphoma cells and displays a highly heterogeneous expression in cancer patients. (A) Lentiviral shRNA-mediated knockdown of ULBP1 and MICA in Molt-4 or Jurkat leukemia cells was confirmed by quantitative RT-PCR using GUSB and PSMB6 as endogenous references. Cells were infected with 10 μL of high-titer virus (107 CFU/mL) in media containing polybrene, submitted to selection 48 hours later, and collected for analysis 96 hours after infection. siSCRAM is an shRNA of scrambled (unspecific) sequence, used as an infection control. Error bars represent SD (n = 3). **P < .01. (B) Molt-4 or Jurkat leukemia cells, subjected to ULBP1 or MICA shRNA knockdown (as in panel A), were used in in vitro killing assays either in the presence (+) or absence (−) of γδ-PBLs (as in Figure 1A). Nontransduced (NT) and siSCRAM-transduced cells were used as controls. (C) Raji lymphoma cells were lentivirally transduced with ULBP1 (or control vector), and surface expression of ULBP1 was assessed by flow cytometry (left). In vitro killing assays were then performed either in the presence (+) or absence (−) of γδ-PBLs (right). (D-E) Quantitative RT-PCR analysis of mRNA expression of NKG2DLs in 8 follicular lymphoma (FL) and 4 diffuse large B-cell lymphoma (DLBCL) biopsies, normalized to housekeeping genes (GUSB and PSMB6) and to a reference sample (reactive follicles) obtained through the same procedure and indicated by the dashed line (D); and in 8 T acute lymphoblastic leukemia (T-ALL) and 7 B acute lymphoblastic leukemia (B-ALL) PBMC samples, normalized to housekeeping genes (GUSB and PSMB6) and to reference PBMCs from healthy persons, indicated by the dashed line (E).
ULBP1 is required for Vγ9Vδ2 T-cell recognition of leukemia/lymphoma cells and displays a highly heterogeneous expression in cancer patients. (A) Lentiviral shRNA-mediated knockdown of ULBP1 and MICA in Molt-4 or Jurkat leukemia cells was confirmed by quantitative RT-PCR using GUSB and PSMB6 as endogenous references. Cells were infected with 10 μL of high-titer virus (107 CFU/mL) in media containing polybrene, submitted to selection 48 hours later, and collected for analysis 96 hours after infection. siSCRAM is an shRNA of scrambled (unspecific) sequence, used as an infection control. Error bars represent SD (n = 3). **P < .01. (B) Molt-4 or Jurkat leukemia cells, subjected to ULBP1 or MICA shRNA knockdown (as in panel A), were used in in vitro killing assays either in the presence (+) or absence (−) of γδ-PBLs (as in Figure 1A). Nontransduced (NT) and siSCRAM-transduced cells were used as controls. (C) Raji lymphoma cells were lentivirally transduced with ULBP1 (or control vector), and surface expression of ULBP1 was assessed by flow cytometry (left). In vitro killing assays were then performed either in the presence (+) or absence (−) of γδ-PBLs (right). (D-E) Quantitative RT-PCR analysis of mRNA expression of NKG2DLs in 8 follicular lymphoma (FL) and 4 diffuse large B-cell lymphoma (DLBCL) biopsies, normalized to housekeeping genes (GUSB and PSMB6) and to a reference sample (reactive follicles) obtained through the same procedure and indicated by the dashed line (D); and in 8 T acute lymphoblastic leukemia (T-ALL) and 7 B acute lymphoblastic leukemia (B-ALL) PBMC samples, normalized to housekeeping genes (GUSB and PSMB6) and to reference PBMCs from healthy persons, indicated by the dashed line (E).
This prompted us to assess the physiologic role of these NKG2DL in leukemia targeting by γδ-PBL through loss-of-function studies using RNA interference. ULBP1 and MICA mRNA and protein expression levels were efficiently and specifically decreased on shRNA infection (Figure 2A; supplemental Figure 2). Loss of ULBP1 expression caused a very significant reduction (35%-50%) of γδ-PBL–mediated lysis of leukemia lines (Figure 2B), essentially “converting” these susceptible tumors into γδ-resistant lines. The residual cytotoxicity may be the result of other NK-like receptors, such as DNAM-1,13 which we are currently investigating. Interestingly, MICA down-regulation did not impair γδ-PBL targeting of these tumors (Figure 2B). These data collectively suggest that ULBP1 plays a crucial and nonredundant role in γδ-PBL recognition of leukemias. Importantly, this constitutes the first physiologic evidence for lymphocyte requirement of NKG2DL expression on tumors because previous studies14,19,21,22 concentrated on their ectopic expression. Along these lines, we have also overexpressed ULBP1 in a resistant lymphoma cell line and observed a marked increase in susceptibility to γδ-PBL cytotoxicity (Figure 2C).
These findings suggest that monitoring ULBP1 levels in leukemia/lymphoma could be of great value in the clinic. In considering this, we analyzed the expression of ULBP1, as well as the other NKG2DL, in 15 leukemia PBMC samples and 12 lymphoma biopsies, which were compared with healthy PBMC and reactive follicles, respectively. ULBP1 presented the highest degree of overexpression in leukemias and lymphomas (Figure 2D-E), as well as the broadest spectrum of expression levels, as translated by its dramatic variance across clinical samples (supplemental Table 3). Taking into account the impact of 2-fold reduction in ULBP1 levels on leukemia killing in vitro (Figure 2A-B), these results with primary biopsies strongly suggest a large variability in susceptibility to γδ-PBL cytotoxicity in the clinical population. We therefore propose ULBP1 to be tested as a biomarker in upcoming γδ T cell–based cancer clinical trials. Moreover, recent findings that proteasome inhibitor drugs specifically up-regulate ULBP1 expression in carcinoma cells23 open new perspectives for cancer immunotherapy.
The expression of ULBP family members correlates with improved survival in cancer patients, and ectopic expression of ULBP1 in particular has been shown to elicit potent antitumor responses.22,24 The role we attribute here to ULBP1 in the context of lymphomas and leukemias is probably not universal for γδ T-cell recognition of other tumor types. For example, susceptible epithelial tumors have been shown to express low or undetectable levels of ULBP1.25 In this context, it is attractive to speculate that ULBP4, recently shown to ectopically trigger Vγ9Vδ2 T-cell cytotoxicity against ovarian and colon carcinomas,14 may play, in epithelial tumors, the equivalent physiologic role of ULBP1 in hematopoietic tumors. This would constitute a novel paradigm for tumor recognition, by which stress-inducible, nonclassic MHC proteins that constitute ligands for NKG2D, would act as cellular reporters of transformation for both circulating Vδ2 and tissue-associated Vδ1 T lymphocytes, the latter known to recognize MICA/MICB and ULBP3.2 Furthermore, NGK2D also plays critical roles in antitumor NK and CD8 T-cell responses5,24 and has been shown to be an essential genetic factor for tumor surveillance in mice.26 We therefore think that NKG2D/NKG2DL modulation entails great promise for cancer immunotherapy.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Serviço de Pediatria do Instituto Português de Oncologia de Lisboa for leukemia samples, Serviço de Anatomia Patológica do Hospital Santa Maria for lymphoma biopsies, M. Eberl for critical reading of the manuscript, A. Hayday and D. J. Pennington for helpful discussions, and P. Simões, D. Saraiva Martins and P. Weinman for technical assistance.
This work was distinguished with the Pfizer Award for Clinical Research 2009. B.S.-S is a European Molecular Biology Organization Installation Grantee. This work was further supported by Fundação para a Ciência e Tecnologia (PTDC/SAU-MII/71662/2006) and Fundação Calouste Gulbenkian (SDH Oncologia 2008; Projecto 99293). L.F.M. is a Young Investigator from the Human Frontier Science Program and was supported by Fundação Luso-Americana para o Desenvolvimento and Fundaçãopara a Ciência e Tecnologia (FCT; PTDC/SAU-MII/69280/2006 and PTDC/SAU-MII/78333/2006). T.L. and D.V.C. received PhD fellowships (47342/2008 and 37898/2007) from FCT.
Authorship
Contribution: T.L., D.V.C., and A.Q.G. performed the experiments; C.F.M., H.R., A.N.-C., C.F., J.S.R., J.T.B., and L.F.M. provided biologic materials and experimental assistance; and B.S.-S. and A.Q.G. designed the study and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Bruno Silva-Santos, Instituto de Medicina Molecular, Avenida Professor Egas Moniz, 1649-028 Lisboa, Portugal; e-mail: bssantos@fm.ul.pt.
References
Author notes
A.Q.G. and B.S.-S. contributed equally to this study.