Abstract
Abstract 99
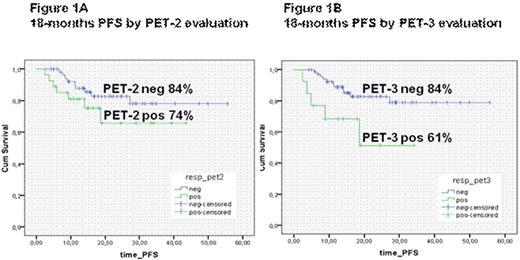
Introduction. The PET scan has a definite role to assess the response at the end of treatment of DLBCL. The evaluation of response by PET after few courses of chemotherapy might be useful to predict chemosensitivity and possibly the outcome in this subset of patients. So far, the predictive value of interim PET in DLBCL pts is still contradictory. The visual analysis of PET results by dichotomous evaluation as positive or negative is often difficult to apply and standardized criteria of interpretation of interim PET have not been established yet. Moreover, published data are often based on retrospective studies, including miscellanea of subtypes and therapies. Our study was aimed to determine the predictive value of interim and final PET on PSF in DLBCL patients. Patients and Methods. From April 2004 to December 2008, 82 newly diagnosed DLBCL patients treated in 5 Hematology Department were included. Clinical features were as follows: median age 56 years (range 19-81); 42 males and 40 females, 29 patients stage I-II and 53 stage III-IV; according to IPI score 47 at low/low-intermediate risk and 35 at intermediate/intermediate-high. All patients were treated according to planned therapy, not modified by PET-2 results, with 6-8 R-CHOP. All patients had PET scan performed at the diagnosis, during treatment (PET-2) and at the end of therapy (PET-3). All PET results were defined as positive or negative by visual dichotomous consensus response criteria. Results. All patients were evaluable for response. PET-2 was performed after 2 R-CHOP in 46 pts, after 3 in 13 and after 4 in 23. At the end of therapy 73 pts (89%) achieved a CR and 9 (11%) were non responders. Fifty-five patients (67%) were negative and 27 (33%) positive at the PET-2 and 69 pts (84%) were negative and 13 (16%) positive at the PET-3. The concordance between clinical CR and PET-3 negativity was 99%: one CR pt was false PET-3 positive due to parothid carcinoma . Correlation between PET results and outcome was evaluated. There was correlation between PET-2 results and CR rate: CR 96% in PET-2 negative pts vs 74% in PET-2 positive (p .004). With a median FU of 18 months, PFS was 78%. PET-2 did not correlate with PFS (p .198): 46/55 (84%) PET-2 negative patients were in CCR and 20/27 (74%) PET-2 positive patients did not progres (Figure 1A). Conversely PET-3 strongly predicted PFS (p .015): 58/69 (84%) were in CCR and 8/13 (61%) did not progressed. (Figure 1B). A further analysis for progression event was performed to adjust the effect of PET-2 analysis for other known risk factors (age up to/over 60, stage, Performance status, LDH, number of extranodal sites, IPI, bulky, Bone Marrow involvement): only LDH (p .005)and IPI 0-2 vs 3-5 (p .001 ) were confirmed as independent predictors of progression event. Conclusions. Our results indicate that in this omogeneous group of DLBCL patients treated with R-CHOP interim PET failed to predict outcome. However, a longer follow up is necessary to validate our data. Conversely PET results at the end of treatment strongly correlate with PFS. Prospective larger studies will be needed to establish the real role of interim PET to predict the outcome in this subset of patients.
Ladetto:CELGENE: Honoraria; JANSSEN-CILAG: Research Funding. Vitolo:Roche: lecture fees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal