Abstract
Allogeneic SCT is currently the preferred therapeutic option for most younger adults with ALL in first complete remission (CR), as recently confirmed by the large ECOG-UKALL Intergroup study (Goldstone, Blood 2008). In this study, however, early response to therapy was not taken into account. As Ig/TCR MRD is one of the main determinants for outcome in childhood ALL, we analyzed its impact on outcome and SCT results in adults treated within pediatric-inspired GRAALL trials. For that purpose, we focused on early MRD evaluations (MRD1: at CR achievement; MDR2: after the first consolidation).
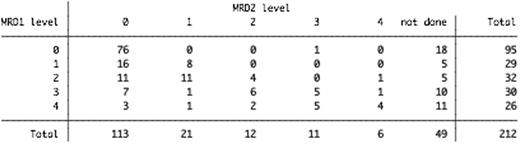
Among 507 patients aged 15-60 years with Ph-negative ALL in first CR after induction included in the GRAALL-2003 (Huguet, JCO 2009) or in the ongoing GRAALL-2005 trial until the first planned interim analysis, 212 patients (B/T lineage, 137/75; median age, 31 years) had an Ig/TCR MDR1 evaluation (with MRD2 evaluation for 77% of them) by CDR3 RQ-PCR or fluorescent competitive Genescan associated with a sensitivity allowing the classification into the following levels: negative (0); positive <10-4 (1); positive 10-4 to 10-3 (2); positive 10-3 to 10-2 (3); positive ≥10-2 (4) (Table 1). Allogeneic SCT was indicated in patients aged 55y or less with a donor (sibling or 10/10 HLA-matched unrelated) and high-risk ALL, as defined on baseline (WBC in B-lineage ALL, CNS involvement, cytogenetics) and response-related risk criteria (steroid- and chemo-sensitivity). Patient characteristics and outcome were identical according to trial, as well as in MRD-tested and non-tested patients.
Cumulative incidence of relapse (CIR) was strongly predicted by 5-level MRD1 (P<0.0001). As CIR were similar in both levels 0-1 and in both levels 3-4, patients were eventually classified as MRD1-fav (level 0-1, N = 124 (59%); 3y-CIR, 13%), MRD1-int (level 2, N = 32 (15%); 3y-CIR, 38%), and MRD1-unfav (level 3-4, N = 56 (26%); 3y-CIR, 56%). Thirty-four of 62 patients at risk reached level 0 or 1 at MRD2 only, 22 of them from the MRD1-int subgroup. However, CIR was not different in these ‘slow responders‘ than in MRD2-int/unfav patients (P=0.27), suggesting that MRD1 alone may be used to stratify further therapy. Median age and baseline characteristics did not differ between MRD1-fav and MRD1-int/unfav patients, while MRD1-fav was associated with higher rates of steroid- and chemo-sensitivity (P=0.05 and P<0.001, respectively). In MDR1-fav patients, 3y-DFS and 3y-OS were 80% (95% CI, 70-87) and 82% (95% CI, 71-90), respectively. After SCT censoring, their 3y-CIR, 3y-DFS, and 3y-OS were 12% (95% CI, 6-24), 84% (95% CI, 72-91), and 86% (95% CI, 72-93), respectively. In multivariate analysis adjusted on protocol, MRD1-fav was the best predictor of lower CIR (RR = 0.22; P<0.001), prolonged DFS (RR = 0.25; P<0.001), and longer OS (RR = 0.20; P<0.001). Low WBC (for CIR, DFS, and OS) and steroid-sensitivity (for CIR only) remained independent risk factors. Similar results were observed in patients with B-lineage ALL, while the number of T-ALL patients was too small to allow a separate analysis. In 127/132 evaluable patients with high-risk ALL eligible for SCT, 3y-CIR was 4% in MRD1-fav and no-donor (N=27), 14% in MRD1-fav and donor (N=33; 30 actually grafted in CR1), 42% in MRD1-int/unfav and donor (N=41; 38 actually grafted in CR1), and 66% in MRD1-int/unfav and no-donor patients (N=26). The difference between donor and no-donor groups tended to be significant in MRD1-int/unfav patients (P=0.14), while not in MRD1-fav patients (P=0.60).
Younger adults with ALL may be classified in a favorable subset with a low relapse rate, only based on post-induction MRD level. At least when treated with a pediatric-inspired protocol, this subset represents more than half patients with Ph-negative ALL. In GRAALL studies, those favorable patients, even when presenting initial bad-risk factors, do not seem to draw any benefit from allogeneic SCT in first CR.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal