Abstract
Abstract 3686
Poster Board III-622
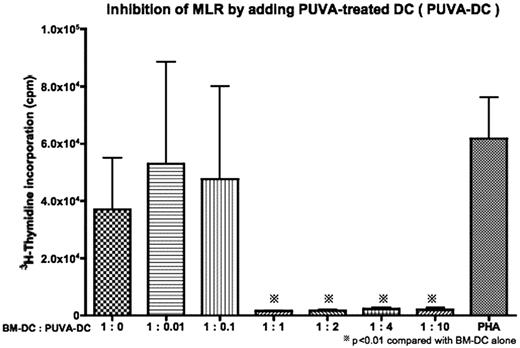
Dendritic cells (DCs) are a heterogenous population of antigen-presenting cells (APCs) that contribute to innate immunity and initiate the adaptive immune response. In addition, recent studies demonstrated the existence of tolerogenic DCs (TDCs) that suppress the immunoreaction. Although the tolerogenic mechanisms are not fully understood, there are some methods reported to generate TDCs from conventional DCs by using cytokines such as IL-10/TGF-beta, vasoactive intestinal peptide (VIP), and IL-21. With the purpose of potential application of TDCs in a clinical bone marrow transplantation for preventing graft-versus-host disease (GVHD), which is caused by strong immunoreaction between host-typed conventional DCs and donor-typed naïve T cells, the establishment of much safer and easier, and more efficient TDCs culture system would be needed. To this end, we investigated whether treatment of conventional DCs with psoralen plus UVA (PUVA), which is widely and safely available in the treatment of some human immune disease and organ transplantation for preventing graft rejection, induced a subset of highly potent TDCs. Bone marrow cells obtained from Balb/c (H-2d) or C57BL/6 (H-2b) were incubated in complete RPMI containing GM-CSF for 10 days to generate bone marrow derived DCs (BM-DCs). BM-DCs were cultured with Psoralen (200 ng/mL) for 30 miniutes and then exposed to UVA light (2J/cm2). After 24 hours UVA irradiation, PUVA-treated DCs were collected and used in all experiments. First, PUVA-treated or untreated DCs with irradiatin were used as stimulator for allogenic splenocytes in mixed leukocyte reactions (MLR). The immunostimulatory capacity of PUVA-treated DCs was significantly diminished compared to those of untreated DCs (p<0.01). The expression levels of CD80 and CD86 by FACS, both of which are costimulatory molecules for T cell activation, was significantly reduced after PUVA treatment (p<0.05). This might explain for the induction of hyporesponsiveness in part. Next we further evaluated whether PUVA-treated DCs directly suppress T cell alloreaciton by cell-to-cell contact. Proliferation was inhibited when PUVA-treated DCs from the stimulator strain were added to the coculture, with a maximum reduction in proliferation of 95% at a 1:1 or higher ratio of untreated DCs to PUVA-treated DCs (Attached file). In conclusion, PUVA-treated DCs directly inhibit T cell alloreaction. Infusion of host-typed PUVA-treated DCs would be potent strategy for preventing lethal acute GVHD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal